Medication Safety: Avoid Dangerous Interactions and Take Drugs Right
When you take a medication safety, the practice of using drugs correctly to avoid harm while getting the intended benefit. Also known as drug safety, it’s not just about following the label—it’s about understanding how your body reacts, what else you’re taking, and when to speak up. Too many people think if a doctor prescribed it, it’s automatically safe. That’s not true. A pill that works perfectly for one person can cause a hospital visit for another—especially when mixed with other drugs, foods, or health conditions.
Drug interactions, when two or more medications affect each other’s action in the body are one of the biggest hidden risks. Take anticoagulants seniors, blood thinners used in older adults to prevent strokes, especially with atrial fibrillation. Many assume falling means they should stop these drugs. But research shows the stroke risk from not taking them is far greater than the bleed risk from a fall. Or consider hypoglycemia risk, the danger of dangerously low blood sugar, often from diabetes medications like sulfonylureas. It’s not just about forgetting to eat—it’s about how those drugs work with alcohol, exercise, or kidney changes as you age.
Even something as simple as prescription dosage instructions, how often and when to take a drug, including terms like 'twice daily' or 'with food' can go wrong. ‘Take with food’ doesn’t mean ‘take with a coffee and a bagel.’ It often means a full meal to slow absorption. Miss that, and you get side effects—or worse, no effect. And don’t assume generics are risk-free. They’re just as effective, but if you switch brands without telling your doctor, your body might not adjust well, especially with narrow-therapeutic-index drugs like warfarin or thyroid meds.
Medication safety isn’t a one-time conversation with your doctor. It’s an ongoing check-in. Did your painkiller start making you dizzy? Did your blood sugar drop after a new antibiotic? Did your sleep pill make you confused? These aren’t normal. They’re signals. The posts below cover real cases—how canagliflozin raises amputation risk, why smoking changes clozapine levels, how NSAIDs and blood thinners can cause internal bleeding, and why some older adults need completely different sleep meds than younger people. You’ll find clear, no-fluff answers on what to watch for, what to ask, and when to say ‘stop.’ This isn’t theory. It’s what actually keeps people out of the ER.
How to Assess Risk When Only Expired Medications Are Available
Expired medications aren't always dangerous, but some can be life-threatening. Learn which drugs are safe to use past their date, which are not, and how to assess risk when no alternatives exist.
Managing Multiple Medications: How to Reduce Drug Interactions and Stay Safe
Managing multiple medications safely means understanding polypharmacy risks, spotting dangerous drug interactions, and working with your healthcare team to deprescribe unnecessary drugs. Learn how to review your meds, reduce side effects, and stay in control.
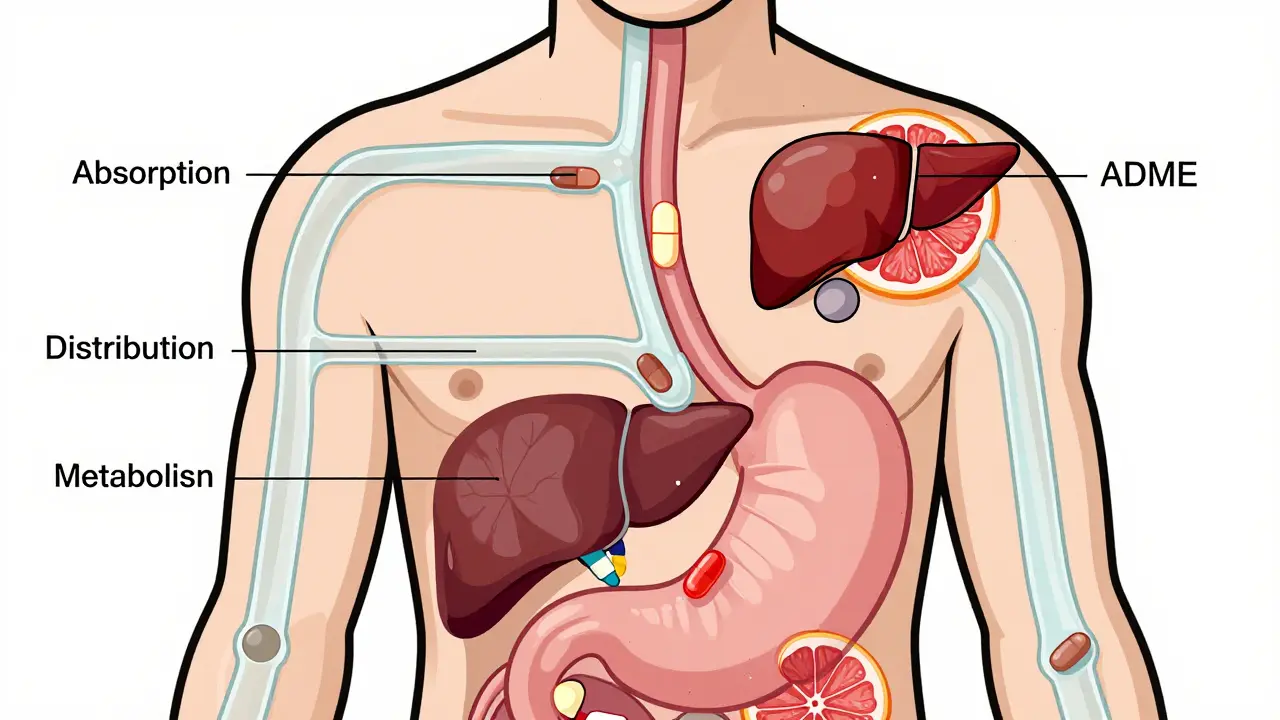
Pharmacokinetic Drug Interactions Explained for Patients: What You Need to Know
Pharmacokinetic drug interactions happen when one medication changes how your body absorbs, breaks down, or removes another. Learn how common drugs, foods, and supplements can cause dangerous effects-and what you can do to stay safe.
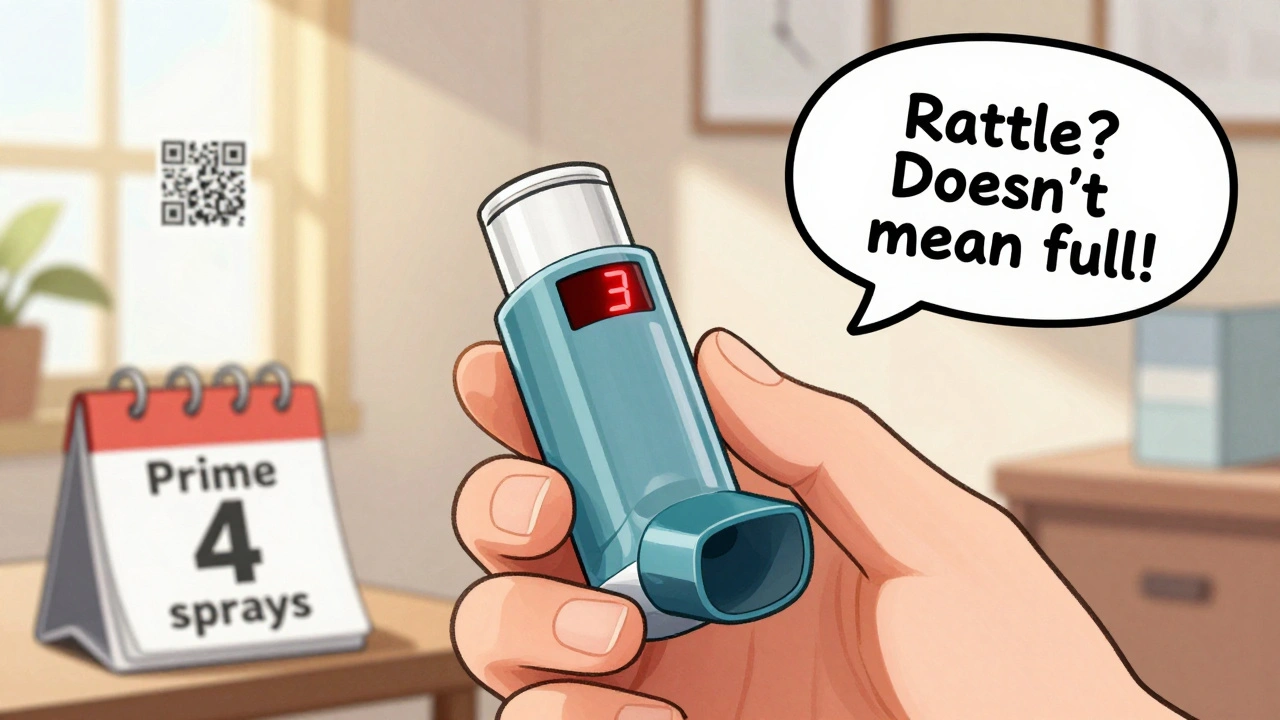
How to Read Prescription Labels for Inhalers, Patches, and Injectables
Learn how to read prescription labels for inhalers, patches, and injectables to avoid dangerous medication errors. Know dosage, concentration, wear time, and safety warnings.
How to Use Patient Counseling to Catch Dispensing Mistakes in Pharmacy Practice
Patient counseling catches 83% of dispensing errors before they reach patients-more than scanners or double-checks. Learn the 4-step method pharmacists use to stop mistakes, who needs it most, and how to make it work under pressure.