
Every year, over 51 million medication errors happen in U.S. pharmacies. Most of them never reach patients-not because of scanners or double-checks, but because a pharmacist asked a simple question: "What is this medicine for?"
That’s the power of patient counseling. It’s not just about giving advice. It’s the last real chance to stop a wrong pill, wrong dose, or wrong instruction before it leaves the pharmacy. And the data doesn’t lie: 83% of dispensing errors are caught during these conversations. That’s higher than barcode scans, higher than pharmacist double-checks, and far cheaper than any tech fix.
Why Patient Counseling Works When Tech Fails
Barcode systems catch about 53% of errors. Pharmacist double-checks catch 67%. But neither can tell if a patient thinks they’re taking a blood pressure pill when it’s actually for diabetes. Or if they’ve never seen this blue capsule before but assume it’s the same as last time.
Patients notice things machines don’t. They know their bodies. They remember what their last prescription looked like. They might say, "This tablet is smaller than usual," or "My doctor said I’d feel dizzy, but this label says it’s for sleep." That’s not a coincidence-it’s a safety net.
The Institute for Safe Medication Practices calls this a "human firewall." No algorithm can replicate the way a patient’s voice, hesitation, or confusion flags a problem. A 90-second chat can cut error rates by nearly half. That’s not theory-it’s from Lumistry’s 2023 analysis of real-world pharmacy data.
The Four-Step Check: What to Ask and When
Effective counseling isn’t random. It’s a system. The American Pharmacists Association recommends a clear 4-step approach that takes just under 3 minutes per patient:
- Verify identity and medication purpose: Don’t ask, "Is this for your blood pressure?" That’s a yes/no trap. Ask, "What condition are you taking this medicine for?" Open-ended questions catch 3.2 times more errors, according to Pharmacy Times. If they say "heart" but the script is for cholesterol, you’ve found a mismatch.
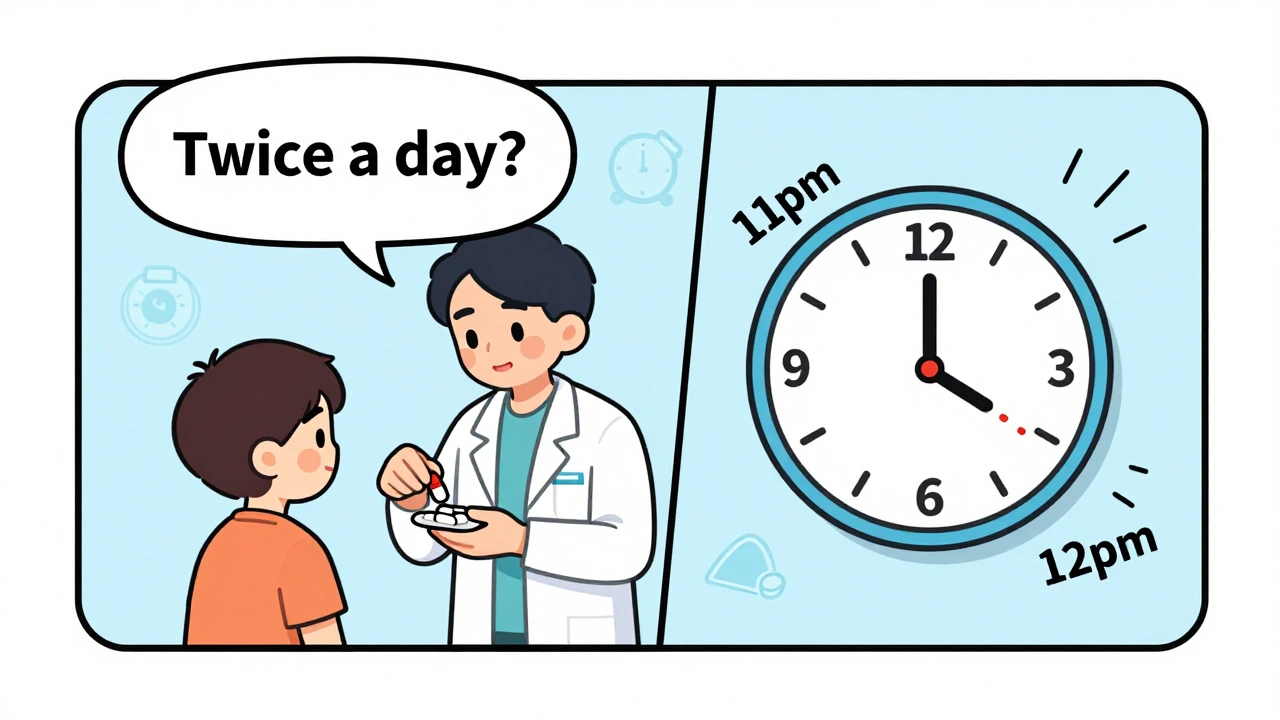
- Check how they’ll take it: Ask them to show you. "Can you demonstrate how you’ll take this?" Many patients don’t know what "take with food" means. Others think "twice daily" means morning and bedtime-when the drug needs to be spaced 12 hours apart. The teach-back method-where the patient explains it in their own words-boosts error detection by 68%.
- Confirm what it looks like: Hold the pill up. Ask, "Does this match what you’ve taken before?" This catches look-alike errors. Insulin pens, opioids, and anticoagulants are especially risky. The National Patient Safety Foundation found that 29% of these errors are caught only when patients recognize the physical change.
- Review interactions and allergies: Ask, "Are you taking anything else?" Don’t assume the electronic record is perfect. Patients forget supplements, OTC meds, or that they started a new antibiotic last week. A single missed interaction can be deadly.
That’s 2 minutes and 40 seconds. The NCBI says you need at least 2.3 minutes to cover all bases. Anything less and you’re leaving safety on the table.
Who Needs It Most-and Why
Not every patient needs the same level of counseling. But some absolutely do:
- Patients over 65: They’re 3.7 times more likely to suffer harm from a dosing error. Memory issues, multiple prescriptions, and changing kidney function make them vulnerable.
- People with low health literacy: One in five patients can’t read beyond a 5th-grade level. They won’t ask questions. They’ll nod and leave. That’s when you need to slow down and rephrase everything.
- New high-alert medications: Insulin, warfarin, opioids, and chemotherapy drugs are the most common sources of serious errors. ISMP reports 1 in 5 dispensing mistakes involve these. Counseling here isn’t optional-it’s critical.
- Patients on 5+ medications: Complex regimens increase error risk by 70%. A simple question like, "Which of these do you take in the morning?" can reveal a mix-up between two similar-sounding drugs.
For routine refills, error detection drops to just 33%. That’s because patients assume nothing changed. But pills change. Manufacturers switch. Generic brands look different. Always ask-even for refills.
Real Stories: What Caught in Counseling
At CVS Health’s 2022 pilot program, pharmacists asked patients: "Does this look like what you’ve taken before?" In three months, they caught 1,247 errors. One was a patient who’d been getting 5mg warfarin for years-but got a 10mg bottle by mistake. She noticed the tablet was larger. Another was a diabetic who received metformin labeled as insulin. She said, "This isn’t clear like my insulin-it’s white and round."
At Walgreens, their "Medication Checkpoint" protocol-where pharmacists show the pill, confirm purpose, and ask teach-back questions-reduced errors by 58% in one year.
One Reddit user shared how their pharmacist caught a dangerous mix-up: "I was given lisinopril instead of losartan. I said, ‘This doesn’t taste the same.’ The pharmacist checked the script-turns out the doctor had changed it, but the pharmacy printed the old one. They apologized, corrected it, and called my doctor. I’ve never been so grateful."
Barriers: Why Counseling Often Falls Short
Despite the evidence, many pharmacies don’t do it right.
Corporate pressure is real. Pharmacists in chain stores report averaging just 1.2 minutes per counseling session-less than half the recommended time. Technicians say they’re told not to "slow down the line." In one survey, 63% said they’re discouraged from spending extra time on counseling.
Staffing is another issue. NCPA found 78% of pharmacies don’t have enough staff to support 3-minute sessions without long waits. But here’s the twist: independent pharmacies, which average 78% counseling compliance, see lower malpractice insurance premiums-19% lower-because they catch more errors.
Documentation matters too. Pharmacies using NABP’s 2022 Counseling Documentation Standards cut liability claims by 44%. If you don’t write it down, it didn’t happen-not in court, not in audit, not in insurance claims.

How to Make It Work in Real Life
You don’t need fancy tech. You need structure.
- Train your team: Use APhA’s Medication Error Prevention Certificate Program. Teach staff to ask open-ended questions, not yes/no traps.
- Use pharmacy technicians: In 42 states, techs can do preliminary counseling under supervision. That frees pharmacists to focus on complex cases.
- Time it: Use a timer. If counseling takes less than 2 minutes, you’re missing something.
- Document it: Use simple checkboxes: Identity confirmed? Purpose verified? Administration understood? Appearance reviewed? Allergies checked?
- Start with high-risk cases: Prioritize new prescriptions, elderly patients, and high-alert drugs. Don’t waste time on routine refills unless something’s changed.
Some pharmacies now use digital tools like Surescripts’ "Counseling Checkpoint" API to log counseling elements right in their workflow. Early adopters say it cuts time by 22% without lowering detection rates.
The Bigger Picture: Safety, Trust, and Savings
Medication errors cost the U.S. healthcare system over $21 billion a year. For a single pharmacy, that could mean $1.7 million in avoided costs just by improving counseling.
CMS now ties 8.5% of Medicare Part D reimbursements to documented counseling that includes error verification. Thirty-four states require counseling for new opioid prescriptions. The proposed 2024 Federal Pharmacy Safety Act could make it mandatory for all high-alert drugs.
Patients notice. In 2023, 89% of reviews on Healthgrades and Yelp praised pharmacies that took time to counsel. One patient wrote: "The pharmacist caught that my new blood thinner was the wrong strength when I said it looked smaller than before. That’s the kind of care I want."
That’s the real win-not just fewer errors, but trust. Patients who feel heard are more likely to take their meds correctly, come back for refills, and recommend your pharmacy.
Technology will keep improving. But the human touch? That’s irreplaceable. The last person to see the medication before it goes home isn’t a scanner. It’s you. And that’s why patient counseling isn’t just good practice-it’s the most powerful tool you have to stop mistakes before they happen.
How long should a patient counseling session last to catch dispensing errors?
Research shows you need at least 2.3 minutes per patient to properly verify medication purpose, administration instructions, physical appearance, and potential interactions. Each additional 30 seconds reduces error rates by 12.7%. A 90-second session can still cut errors by nearly half, but 3 minutes is the gold standard for full safety coverage.
Is patient counseling more effective than barcode scanning?
Yes. Barcode scanning catches about 53% of dispensing errors. Pharmacist double-checks catch 67%. But patient counseling catches 83%-because it verifies not just the physical medication, but the patient’s understanding and expectations. Machines can’t detect if a patient thinks they’re taking a blood pressure pill when it’s actually for diabetes.
What type of questions catch the most errors during counseling?
Open-ended questions catch 3.2 times more errors than closed ones. Instead of asking, "Is this for your blood pressure?" ask, "What condition are you taking this medicine for?" This forces the patient to explain in their own words, revealing misunderstandings or mismatches. The teach-back method-where patients repeat instructions back to you-is especially powerful, increasing detection by 68%.
Why is counseling less effective for routine refills?
Patients assume nothing has changed. But pills can change-different manufacturers, sizes, colors, or even active ingredients. For refills, error detection drops to just 33%. Always ask, "Does this look like your last bottle?" even if it’s the same medication. A change in appearance is one of the most common red flags.
Can pharmacy technicians help with patient counseling?
Yes. In 42 states, pharmacy technicians are allowed to perform preliminary counseling under pharmacist supervision. They can verify identity, ask about medication purpose, and check for allergies. The pharmacist then reviews and confirms. This boosts effective counseling time by 37% and helps manage workload without sacrificing safety.






8 Comments
It's wild how we've outsourced human judgment to machines and then act surprised when they fail. The real magic isn't in the barcode or the double-check-it’s in the moment someone looks you in the eye and asks, 'What's this for?' That’s not protocol. That’s compassion with a purpose. We treat healthcare like a transaction, but healing? Healing needs conversation.
lol so u mean the gov and big pharma dont want u talkin to pharmacists? 😏 they prolly got a secret agenda-like makin sure u stay sick so u keep buyin pills. i heard the blue capsules are actually mind control chips. also, why do all the studies say 'lumistry'-is that a company or a cult? 🤔
83%? That’s garbage. You’re just cherry-picking data. Most of those 'errors' are just patients being dumb. They think aspirin is for headaches and not heart disease. That’s not the pharmacy’s fault. And 3 minutes? No way. I’ve seen pharmacies do it in 45 seconds and still catch stuff. This whole thing is overblown.
This made me cry 😭 Seriously-thank you for saying this. I had a pharmacist stop me last week and ask, 'Does this look right?' I said no, it was smaller. Turns out they gave me the wrong strength. She didn’t just fix it-she sat with me for 10 minutes and explained everything. I’ve never felt so seen in a pharmacy before. 🙏❤️
Let’s be honest: if your pharmacy requires a 3-minute counseling session, you’re operating at a 1998 efficiency level. The real innovation is in AI-driven predictive analytics that cross-references patient history, genetic markers, and drug interaction databases. What you’re advocating is a nostalgic throwback to manual labor-fine for small-town clinics, but utterly unsustainable in modern healthcare systems. The future is automated, not interpersonal.
Stop pretending this is optional. If you’re not documenting every counseling interaction using NABP standards, you’re not just negligent-you’re endangering lives. And if your pharmacy tells you to 'speed up the line,' that’s not a business decision-it’s malpractice waiting to happen. I’ve seen patients die because someone skipped the 'What is this for?' question. Don’t make excuses. Do the work.
I work in a rural clinic. We don’t have fancy tech. We don’t have time. But we do have patience. One elderly lady came in for her blood pressure med and said, 'This pill tastes different.' We checked-she was right. It was a new generic. She’d been on the old one for 12 years. She didn’t know the name, didn’t know the dose-but she knew how it tasted. That’s the kind of knowledge no algorithm can replicate. We just listen. And sometimes, that’s enough.
THIS. IS. EVERYTHING. 🚨 I used to think tech was the future-until I saw a pharmacist catch a lethal insulin mix-up because a 78-year-old man said, 'This pen feels lighter.' That’s not luck. That’s skill. That’s humanity. If your pharmacy doesn’t train staff to treat counseling like a sacred ritual-not a checkbox-you’re not a pharmacy. You’re a vending machine with a white coat. Wake up. The system’s broken. And the fix? It’s right in front of you-in the patient’s voice.