LDAA Dose Calculator
This calculator helps determine if you qualify for Low-Dose Azathioprine with Allopurinol (LDAA) therapy based on your metabolite levels. Enter your clinical values to see if LDAA might be appropriate for you.
Enter your metabolite values to see results.
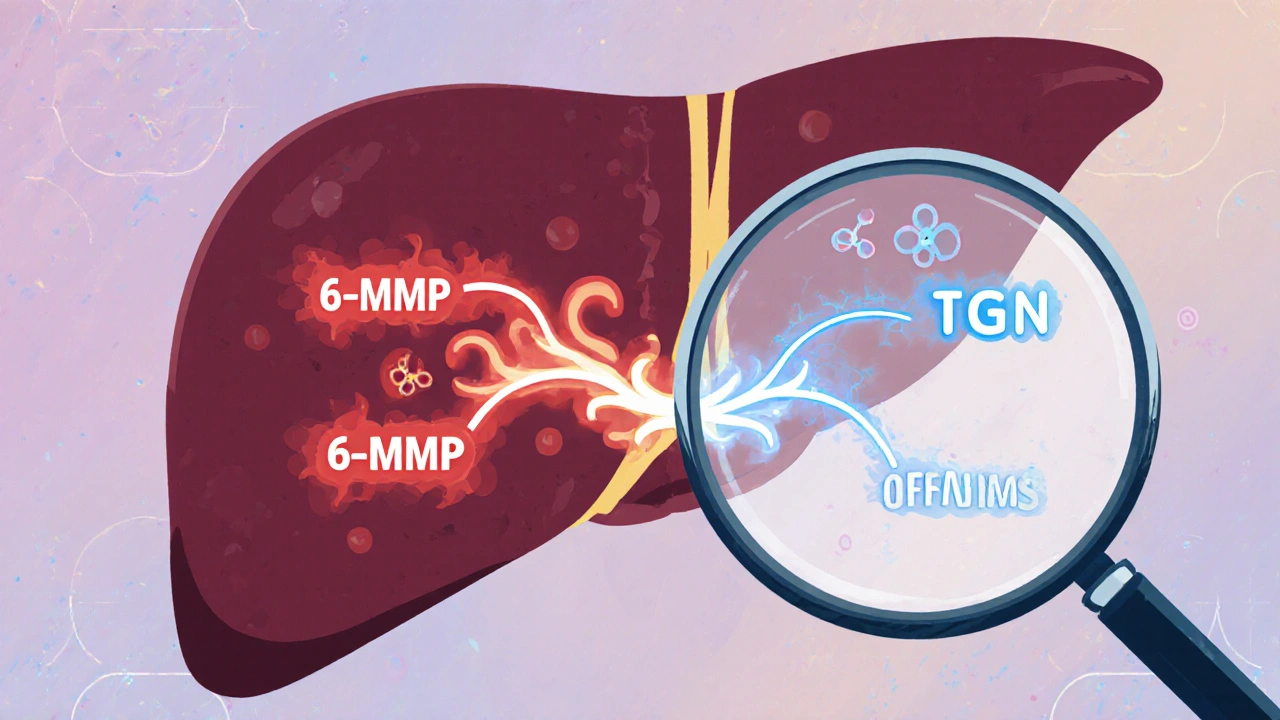
When azathioprine doesn’t work-or makes you sicker-it’s not always the drug’s fault. It’s often how your body breaks it down. For some people, azathioprine turns into too much of a toxic byproduct called 6-MMP, which damages the liver but does little to calm inflammation. Meanwhile, the good stuff-6-TGN, the metabolite that actually suppresses the immune system-stays too low. That’s where allopurinol comes in. Used for decades to treat gout, allopurinol has become an unexpected lifeline for patients stuck on failing azathioprine therapy. Together, they form what’s now called LDAA (low-dose azathioprine with allopurinol), a strategy that flips the script on thiopurine metabolism and saves lives.
Why Azathioprine Alone Fails for Some People
Azathioprine has been around since the 1960s. It’s cheap, widely available, and used for Crohn’s disease, ulcerative colitis, autoimmune hepatitis, and even after organ transplants. But it doesn’t work the same way for everyone. About 15-20% of patients are "hypermethylators," meaning their bodies convert too much azathioprine into 6-MMP instead of 6-TGN. These patients often have normal or even high levels of the enzyme TPMT, which drives this unwanted pathway. The result? Liver enzymes spike, nausea and fatigue set in, and the disease keeps flaring. Doctors see this all the time: patients on full-dose azathioprine for months with no improvement, then told to switch to expensive biologics-when a simpler fix might be hiding in plain sight.How Allopurinol Changes Everything
Allopurinol blocks an enzyme called xanthine oxidase. That’s why it works for gout-it stops uric acid from forming. But in the context of azathioprine, blocking xanthine oxidase does something unexpected: it forces the drug down a different metabolic path. Instead of being turned into 6-MMP or broken down into useless 6-thiouric acid, more of the drug gets converted into 6-TGN. Studies show this shift can increase 6-TGN levels by 2 to 5 times while slashing 6-MMP by 70-90%. That’s not a small tweak. It’s a complete metabolic overhaul. But here’s the catch: you can’t just add allopurinol to a full dose of azathioprine. That’s how people ended up in the hospital in the 1980s-with dangerously low white blood cell counts. The fix? Cut azathioprine to 25-33% of the usual dose. So if someone was taking 150 mg/day, they drop to 50 mg/day and add 100 mg of allopurinol. That’s the LDAA protocol. And when done right, it’s incredibly effective.Who Benefits Most From LDAA?
LDAA isn’t for everyone. It’s targeted. The best candidates are patients who:- Have high 6-MMP levels (>5,700 pmol/8×10⁸ RBCs)
- Have low 6-TGN levels (<230 pmol/8×10⁸ RBCs)
- Have elevated liver enzymes despite taking azathioprine
- Have normal or high TPMT activity (above 14.2 U/mL)

The Risks: Why Monitoring Is Non-Negotiable
LDAA isn’t risk-free. If you don’t reduce the azathioprine dose, you’re asking for trouble. The same mechanism that boosts 6-TGN also increases the risk of myelosuppression-low white blood cells, low platelets, anemia. Early studies without dose adjustments reported leukopenia in up to 40% of patients. Today, with strict protocols, that number is under 10%, but only if you follow the rules. The guidelines are clear: check your complete blood count weekly for the first four weeks, then every two weeks. If your absolute neutrophil count drops below 1.5 × 10⁹/L, hold the azathioprine. Most patients bounce back after a short break. Permanent discontinuation is rare-only about 10% of cases. You also need to test for TPMT deficiency. If your TPMT is very low (<5 U/mL), you’re at high risk for severe bone marrow suppression even with low doses. LDAA won’t help you. You need a different drug entirely-maybe 6-mercaptopurine at a microdose, or a biologic.Real Stories: Success and Near-Misses
On patient forums, the stories are powerful. One user on r/IBD wrote: "After three years of failed Humira and full-dose azathioprine with liver enzymes through the roof, I went on 50 mg azathioprine + 100 mg allopurinol. Liver enzymes normalized in 8 weeks. I’ve been in remission for 14 months. No side effects." But there are warning signs too. Another user posted: "Went on LDAA without monitoring. Neutrophils dropped to 0.8 in three weeks. Hospitalized for fever. Now I’m terrified of all immunosuppressants." The difference? Monitoring. The first patient had a doctor who knew the protocol. The second didn’t. That’s the line between life-changing relief and a medical emergency.How It Compares to Biologics
Biologics like infliximab or adalimumab are effective-but they cost $30,000 to $50,000 a year. LDAA? Around $1,200-$1,800. That’s a 20-to-1 difference. In Europe, 65% of IBD centers now use LDAA as a second-line option. In the U.S., adoption is slower, partly due to outdated fears from the 1980s. But guidelines have changed. The European Crohn’s and Colitis Organisation (ECCO) and the American Gastroenterological Association (AGA) both now recommend LDAA for azathioprine-intolerant patients. It’s not just about cost. For patients who’ve failed biologics or can’t tolerate them, LDAA offers a chance to get back on track with an old drug made new.What Doctors Need to Know
Starting LDAA isn’t complicated, but it requires precision:- Test TPMT activity and thiopurine metabolites (6-TGN and 6-MMP) before starting.
- Reduce azathioprine to 50 mg/day (or 25-33% of original dose).
- Add allopurinol 100 mg/day.
- Check CBC weekly for 4 weeks, then every 2 weeks.
- At 4 weeks, retest metabolites: aim for 6-TGN 230-450 pmol/8×10⁸ RBCs and 6-MMP below 2,800 pmol/8×10⁸ RBCs.
The Future of LDAA
New tools are coming. Two companies are developing rapid point-of-care tests to measure thiopurine metabolites in under an hour. Right now, you need to send blood to a specialized lab, and results take days. With faster testing, doctors could adjust doses in real time-like tuning a car engine while it’s running. LDAA is also being tested in autoimmune hepatitis. A 2023 study showed 82% of patients who failed standard therapy went into remission with LDAA. That’s huge. It’s no longer just an IBD trick-it’s becoming a broader tool for autoimmune disease.Bottom Line
Azathioprine and allopurinol together aren’t a magic bullet. But for the right patient, they’re one of the most powerful, underused tools in gastroenterology. The key isn’t just combining two drugs-it’s understanding the chemistry behind them. When you know how 6-MMP and 6-TGN compete, you can steer metabolism in the right direction. And that’s how you turn a failing drug into a lifesaver.Can I take azathioprine and allopurinol together without reducing the azathioprine dose?
No. Taking full-dose azathioprine with allopurinol can cause severe, life-threatening bone marrow suppression. The azathioprine dose must be reduced to 25-33% of the original amount (typically 50 mg/day) when adding allopurinol. This is non-negotiable and based on multiple clinical studies.
Is LDAA safe for people with kidney problems?
No. LDAA is contraindicated in patients with severe renal impairment (creatinine clearance below 30 mL/min). Allopurinol and its active metabolite, oxypurinol, are cleared by the kidneys. In kidney failure, these drugs build up and increase the risk of toxicity. Dose adjustments aren’t enough-avoid the combination entirely in this group.
What if my TPMT level is low?
If your TPMT activity is below 5 U/mL, you have a genetic deficiency that makes you extremely sensitive to thiopurines. LDAA will not help you-it will likely cause dangerous bone marrow suppression. You should avoid azathioprine entirely and use alternative therapies like biologics or methotrexate.
How long does it take to see results with LDAA?
Liver enzymes usually improve within 4-8 weeks. Clinical improvement in symptoms like diarrhea, pain, or fatigue can take 8-12 weeks. Metabolite levels should be checked at 4 weeks to confirm the right balance of 6-TGN and 6-MMP. Don’t expect instant results-this is a slow, precise adjustment.
Is LDAA covered by insurance?
Yes. Both azathioprine and allopurinol are generic, low-cost drugs. Most insurance plans cover them with minimal copays. The total annual cost is typically under $2,000, making it far cheaper than biologics. Some insurers may require prior authorization for allopurinol when used off-label, but this is usually granted when supported by metabolite testing.
Can LDAA be used for autoimmune hepatitis?
Yes. A 2023 study in Hepatology showed that 82% of patients with autoimmune hepatitis who failed standard azathioprine therapy achieved remission with LDAA. It’s now being considered as a standard option for patients who can’t tolerate or respond to conventional doses.






8 Comments
This is such a game-changer for IBD patients who’ve been stuck on azathioprine with no results. I’ve seen friends go from liver enzymes through the roof to feeling like themselves again in just a few weeks. It’s wild how a gout drug became a miracle fix for autoimmune stuff. Why isn’t this protocol standard everywhere?
The pharmacokinetic rationale for LDAA is well-supported in the literature, particularly in studies from the early 2010s. The inhibition of xanthine oxidase redirects metabolic flux toward thioguanine nucleotides, thereby enhancing therapeutic efficacy while reducing hepatotoxicity. However, monitoring of complete blood counts remains essential during initiation.
OMG YES. My cousin was on 150mg azathioprine for 2 years, liver fried, still had flares. Doctor finally tried the low-dose + allopurinol thing and boom-her 6-MMP dropped to normal, 6-TGN went up, and she’s been in remission for 18 months. No biologics, no $$$, no hospital visits. India’s doing this too now, but docs still don’t know about it. Spread the word!
This is incredible! Seriously, this is one of those rare, beautiful moments in medicine where a cheap, old drug, used for something totally different, fixes a problem that expensive new drugs can’t! I’m so glad this is getting attention! Please, please, please-do not skip the lab monitoring! Always check your 6-TGN and 6-MMP levels before and after! And don’t just guess the dose-work with a gastroenterologist who knows thiopurine metabolism! This could save your life!
wait so allopurinol is basically like… a drug wizard? like it’s not just for gout, it’s like a metabolic switch? i mean… what if all drugs are just… misunderstood? like maybe aspirin’s real purpose is to make you cry in the shower? and we just got lucky? also, is this why my dog stopped licking his balls after i gave him my leftover meds? just sayin’
Who’s really funding this ‘LDAA’ hype? Big Pharma doesn’t want you to know that two cheap, generic drugs can replace their $100,000/year biologics. This isn’t science-it’s a conspiracy. They’ve been poisoning us with azathioprine for decades so we’d keep buying their expensive treatments. Now they’re quietly pushing allopurinol as a ‘solution’ to look like heroes while keeping the profit pipeline alive. Check the patent filings. Look at the clinical trial sponsors. It’s all connected. Wake up.
While I appreciate the clinical observations presented, I must emphasize that the absence of long-term, randomized, double-blind, placebo-controlled trials-particularly those with stratified genetic analysis of TPMT and NUDT15 polymorphisms-renders this approach premature at best, and potentially hazardous at worst. The ethical implications of off-label metabolic manipulation without comprehensive pharmacogenomic screening are, frankly, unconscionable.
LDAA is not a novel concept. It was first described in 1998 by Prof. S. R. B. in the journal Gut. The 25–33% azathioprine dose reduction with concurrent allopurinol is standard of care in the UK and Australia since 2012. Any clinician unfamiliar with this protocol is either negligent or inadequately trained. Furthermore, 6-MMP levels above 5,700 pmol/8×10⁸ RBCs are not merely ‘high’-they are unequivocally pathological and require intervention. This post undersells the evidence.