Every year, thousands of people die not from taking one drug, but from mixing them. It’s not about being reckless-it’s often about not knowing. A person takes their prescribed painkiller, has a drink at dinner, and doesn’t realize they’re playing Russian roulette with their breathing. Or someone uses cocaine to stay alert, then adds heroin to calm down, not knowing the combination creates a toxin in their liver that’s more deadly than either drug alone. These aren’t rare mistakes. They’re common, preventable, and deadly.
Why Mixing Drugs Is More Dangerous Than You Think
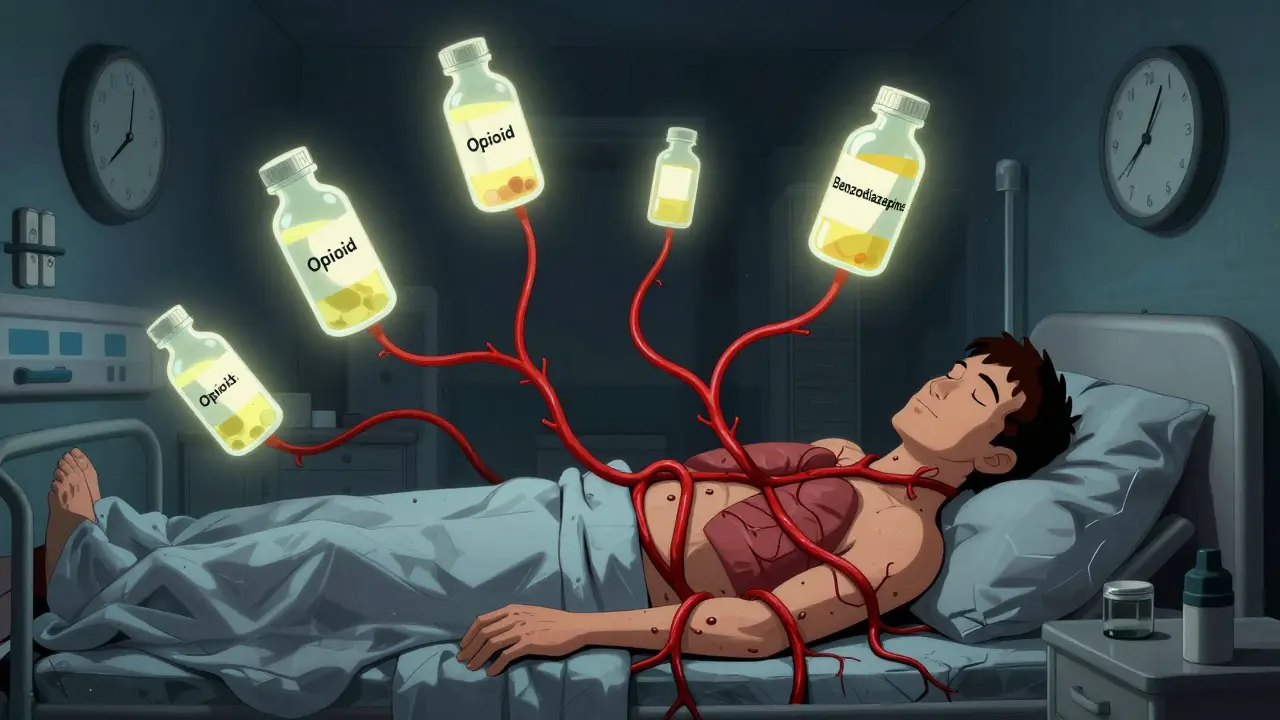
Drugs don’t just add up-they multiply. When two or more substances enter your body at the same time, they don’t just coexist. They interact. Some interactions make the effects stronger. Others create entirely new, toxic compounds. The body wasn’t designed to handle these combinations. Your liver gets overwhelmed. Your brain loses control of breathing. Your heart goes into chaos. The most dangerous interactions happen between drugs that affect the same system. Central nervous system (CNS) depressants-like opioids, benzodiazepines, alcohol, and barbiturates-are especially risky when mixed. They all slow down your brain and breathing. When you combine them, your body doesn’t just slow down a little. It can shut down completely.The Deadliest Combo: Opioids + Benzodiazepines
If you’re taking an opioid like oxycodone, hydrocodone, or fentanyl for pain, and you’re also prescribed a benzodiazepine like Xanax, Valium, or Ativan for anxiety or sleep, you’re in a high-risk zone. The CDC found that in 2020, 30.1% of opioid-related overdose deaths also involved benzodiazepines. That’s more than one in three. These drugs work together to suppress your respiratory drive. Alone, an opioid might slow your breathing to 8 breaths per minute. Add a benzodiazepine, and it can drop to 4 or even 2. You might not even realize you’re in danger until it’s too late. There’s no warning sign like a pounding headache or sweating. You just stop breathing. Even if you’re taking your medications exactly as prescribed, mixing them can be deadly. That’s why Medicare Part D started requiring electronic alerts in 2019 when doctors try to prescribe both together. Since then, concurrent prescribing has dropped by 18%. But millions still get both prescriptions. If you’re on either, ask your doctor: “Could this interact with my other meds?”Opioids + Alcohol: A Silent Killer
Alcohol is the most commonly mixed substance with opioids-and one of the most dangerous. The National Institute on Alcohol Abuse and Alcoholism (NIAAA) says alcohol-medication interactions cause about 20% of all emergency visits for adverse drug events. When you mix alcohol with opioids, the sedative effects don’t just add up-they multiply. Research shows this combo increases the risk of respiratory depression by 4.5 times compared to opioids alone. That means if you normally feel drowsy after taking your painkiller, alcohol turns that into a coma risk. Even one drink can be enough. A Reddit user shared how two beers after dental surgery with oxycodone led to respiratory arrest. They needed naloxone to survive. That’s not an outlier. It’s a pattern. The SA Health Department says: “The more alcohol in your body, the less heroin you need to cause an overdose.” The same applies to prescription opioids.
The Speedball: Cocaine + Heroin
This combo has a chilling nickname: the speedball. It’s a stimulant and a depressant, meant to balance each other out. But instead of canceling danger, they amplify it. Cocaine speeds up your heart, raises your blood pressure, and makes you feel invincible. Heroin slows your breathing and makes you feel calm. Together, they create a dangerous push-pull effect. Your heart races while your lungs struggle. Blood pressure spikes to dangerous levels-often over 180/110. Heart rate can hit 160 beats per minute. Worse, your liver turns cocaine and alcohol into a new toxin called cocaethylene. This compound lasts longer in your body than cocaine alone and is 25% more likely to cause sudden death. It also damages your liver, weakens your immune system, and increases seizure risk. Studies show 65% of chronic users of this combo suffer liver toxicity. This combination has killed celebrities like John Belushi, River Phoenix, and Chris Farley. But most deaths go unreported. The CDC found that in 2021, nearly half of all cocaine overdoses involved heroin. It’s not a myth. It’s a death sentence.Antidepressants + Alcohol: A Hidden Risk
Many people think it’s safe to have a drink while on antidepressants. It’s not. Drugs like duloxetine (Cymbalta) and venlafaxine (Effexor) already stress your liver. Add alcohol, and that stress becomes damage. A 2018 study found that mixing alcohol with duloxetine increases liver toxicity risk by 40%. With venlafaxine, alcohol lowers the threshold for fatal overdose by 25%. That means if you normally could handle six drinks without harm, taking venlafaxine might make three drinks deadly. The symptoms aren’t always obvious. You might feel more tired than usual. Your stomach might hurt. You might feel dizzy. These aren’t just side effects-they’re early signs your liver is failing.Buprenorphine + Alcohol: A Trap for Recovery
Buprenorphine is used to treat opioid addiction. It’s safer than methadone and helps people stay off heroin. But mixing it with alcohol is a major red flag. This combo can cause severe hypotension-blood pressure dropping below 90/60. It can slow breathing to fewer than 10 breaths per minute. It can cause profound sedation, confusion, and coma. People in recovery often think, “I’m not using heroin anymore, so a drink won’t hurt.” But buprenorphine still depresses your central nervous system. Alcohol turns it into a trap.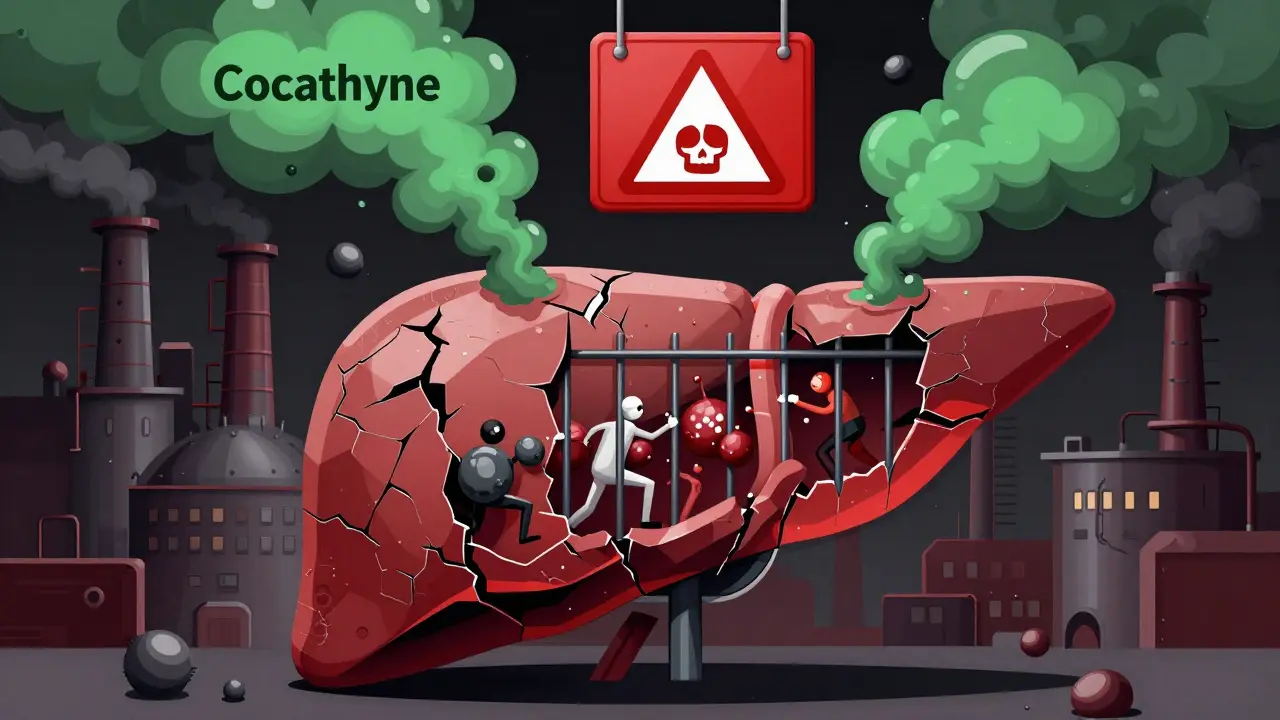






14 Comments
This post is spot-on. Mixing drugs is a dumbass gamble with your life, and nobody talks about it enough.
People think they’re ‘in control’-until their liver starts screaming and their brain forgets how to breathe. It’s not a party trick. It’s a slow-motion suicide with a side of denial. And the worst part? They’ll post memes about it tomorrow while their family scrambles to find their body. I’ve seen it. Too many times. Don’t be the statistic. Don’t be the ‘oh, I’ve done it before’ ghost.
It's fascinating how society normalizes the ingestion of chemicals as if we're all just lab rats in a corporate experiment, you know? We're told to take pills for everything-sleep, anxiety, pain-then we're expected to magically know which ones won't kill us when combined with wine or coke or whatever’s on the table. But the system doesn't care. It's profit-driven, not safety-driven. The real red flag isn't the drug combo-it's the fact that we're allowed to be this ignorant in the first place. The body isn't a vending machine. You can't just insert two coins and expect one snack. You get a bomb.
I lost my brother to this. He took his prescribed oxycodone after a few drinks because he said ‘it helped him relax.’ No one warned him. No one told him it wasn’t just ‘a little sleepy.’ He just… stopped. I wish someone had printed this post and taped it to his bathroom mirror.
Thank you for writing this. I’ve been on antidepressants for years and never realized a single glass of wine could be dangerous. I’m going to talk to my doctor tomorrow. You’re right-it’s not about fear. It’s about awareness. And awareness saves lives.
Stop pretending you’re safe because you ‘only do it on weekends.’ Your liver doesn’t care about your schedule. Your heart doesn’t care if you’re ‘responsible.’ You’re not a superhero-you’re a walking overdose waiting to happen. Get help. Or get out of the way of people who actually want to live.
My uncle died this way. No one told him. Please share this.
If you're taking any medication, especially for mental health or chronic pain, please-please-ask your pharmacist. They’re the unsung heroes who know your full history. I’ve seen them catch deadly interactions before they happen. Don’t skip that step.
Why do Americans think they’re immune to this? In India, we know alcohol + painkillers = death. We don’t need a CDC report to tell us that. You people act like this is new news. It’s not. You’re just now waking up.
My mom’s on buprenorphine and drinks wine every night. I showed her this. She cried. Then she stopped. I’m not trying to be preachy-I just don’t want to lose her. Thank you for saying what I couldn’t.
CNS depressant synergism + hepatic enzyme inhibition = lethal pharmacokinetic cascade. This isn’t anecdotal. It’s biochemistry.
So… if I take my Xanax and then have a beer… am I basically doing a science experiment with my own death? Cool. Got it.
This is all fearmongering. People have been mixing drugs since the dawn of time. If you can’t handle it, don’t do it. But don’t lecture the rest of us like we’re children. The body adapts. You think you’re saving lives? You’re just policing autonomy.
Luke, you’re not helping. This isn’t about ‘autonomy’-it’s about people dying because no one told them. You don’t get to be ‘edgy’ while someone’s kid is on a ventilator because they thought ‘one drink won’t hurt.’ This isn’t a debate. It’s a funeral.