When you take more than one medication, your body doesn’t just treat them separately. One drug can change how another works-sometimes in ways that are dangerous, sometimes in ways you won’t even notice. These changes are called pharmacokinetic drug interactions. They don’t mean the drugs are fighting each other directly. Instead, they’re about how your body moves, breaks down, and gets rid of each medicine. Understanding this can keep you safe.
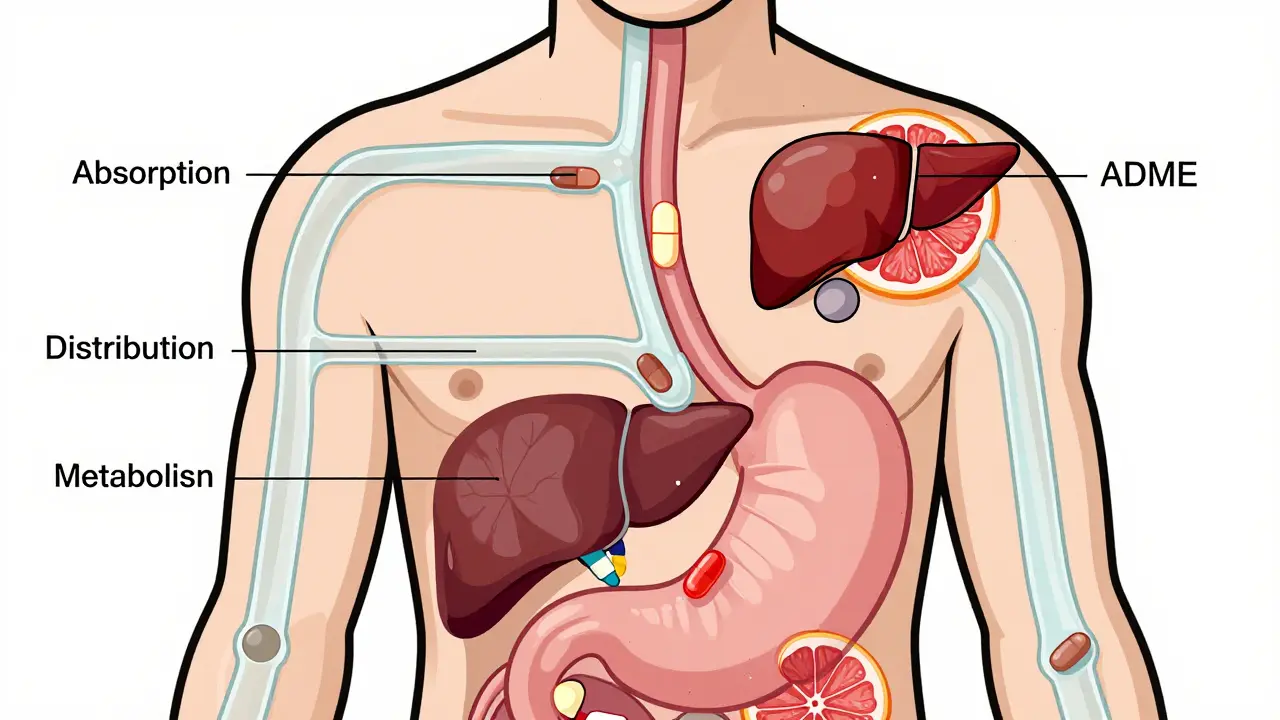
How Your Body Handles Drugs: The ADME System
Your body processes every drug through four main steps: Absorption, Distribution, Metabolism, and Excretion. Scientists call this ADME. If one drug messes with any of these steps for another drug, that’s a pharmacokinetic interaction.
Let’s say you take a painkiller and an antibiotic at the same time. One might slow down how fast the other gets into your blood. Or it might stop your liver from breaking it down. That means more of the drug stays in your system than it should. Too much can cause side effects. Too little means it won’t work.
Absorption: When Drugs Don’t Get Into Your Blood Properly
Some drugs need your stomach to be acidic to be absorbed. If you take an antacid for heartburn right before your thyroid medicine, the antacid neutralizes the acid. That means your thyroid pill won’t absorb well. You might not feel its effects at all.
Another common issue happens with dairy and antibiotics. If you take tetracycline or ciprofloxacin with milk, yogurt, or cheese, the calcium in those foods binds to the antibiotic. This stops it from being absorbed. Studies show this can cut the amount of drug your body gets by up to half. The fix? Wait at least two to three hours between dairy and these antibiotics.
Even something as simple as food can matter. Opioids like morphine slow down your gut, which delays how quickly pain relievers like acetaminophen get absorbed. That means your pain relief might come later than expected.
Distribution: When Drugs Compete for Space in Your Blood
Once drugs get into your bloodstream, they often stick to proteins like albumin. Think of it like a bus-there’s only so much room. If two drugs want to ride the same bus, one might push the other off.
This is most dangerous with drugs that have a narrow safety window. Warfarin, for example, is used to prevent blood clots. If you take diclofenac (a common painkiller) with it, diclofenac can push warfarin off the protein. Suddenly, more warfarin is floating around freely in your blood. That increases your risk of serious bleeding.
But here’s the catch: this kind of interaction doesn’t always cause problems. Your body often adjusts by breaking down the extra free drug faster. That’s why it’s rare to see big issues unless the drug is already risky-like warfarin, digoxin, or phenytoin.

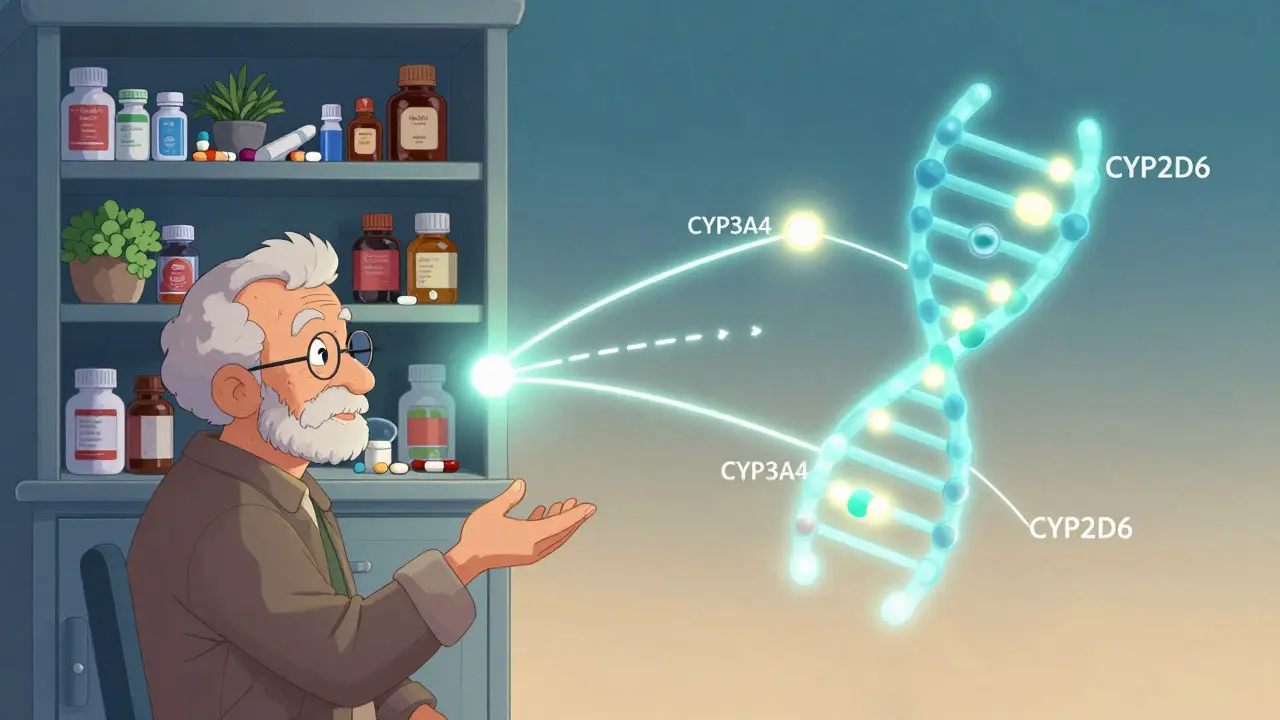
Metabolism: The Most Dangerous Type of Interaction
This is where things get serious. Most drugs are broken down in your liver by enzymes called cytochrome P450 (CYP). The two biggest players are CYP3A4 and CYP2D6. If one drug blocks or speeds up these enzymes, it changes how fast other drugs are cleared from your body.
Inhibitors slow down metabolism. Grapefruit juice is the most famous example. It blocks CYP3A4. That means if you’re taking a statin like simvastatin, or a blood pressure drug like felodipine, your body can’t break them down. Levels build up. You could get muscle damage, low blood pressure, or even heart rhythm problems.
Other common inhibitors include cimetidine (an old heartburn drug), fluoxetine (Prozac), and clarithromycin (an antibiotic). One study showed that when clarithromycin was taken with midazolam (a sedative), midazolam levels jumped so high that patients became dangerously sleepy or had trouble breathing.
Inducers do the opposite-they make your liver break down drugs faster. St. John’s Wort, used for mild depression, is a powerful inducer. It can make birth control pills fail, reduce the effect of antidepressants, or even cause organ transplant patients to reject their new organ by lowering immunosuppressant levels.
Another example: phenobarbital, used for seizures, can speed up the breakdown of lamotrigine (another seizure drug). In some cases, this causes toxic byproducts to form, leading to low blood cell counts-a serious condition called leukopenia or thrombocytopenia.
According to the FDA, about 60% of all approved drugs interact with CYP enzymes. That’s not rare. It’s normal.
Excretion: When Your Kidneys Get Overloaded
Your kidneys help flush drugs out of your body. But if two drugs use the same cleanup pathway, they can clog it.
Probenecid, used for gout, blocks the kidney’s ability to get rid of certain antibiotics like cephalosporins. That means the antibiotic stays in your system longer. It might work better-but it could also cause side effects like nausea or kidney stress.
NSAIDs like ibuprofen or naproxen can interfere with methotrexate, a drug used for arthritis and some cancers. When they’re taken together, methotrexate builds up. That can lead to bone marrow suppression, making it harder for your body to make blood cells.
Then there’s P-glycoprotein, a transporter that pushes drugs out of your kidney and gut cells. Drugs like digoxin (used for heart rhythm) rely on this system. If you take it with itraconazole (an antifungal), the transporter gets blocked. Digoxin levels rise. You could develop a dangerous heart rhythm called ventricular tachycardia.
The FDA says about 20% of serious drug interactions involve transporter proteins like this. It’s not just about the liver anymore.
Real Risks: What Happens When Things Go Wrong
These aren’t theoretical. People get hospitalized because of these interactions.
One case involved an 85-year-old woman taking venlafaxine (an antidepressant) and propafenone (a heart rhythm drug). Both are processed by CYP2D6 and blocked by P-glycoprotein. Together, venlafaxine levels spiked. She developed hallucinations and agitation. Her doctors had to stop one drug and adjust the other.
Another case: a patient on warfarin started taking an antibiotic that inhibited its breakdown. Their INR (a blood clotting test) jumped from 2.5 to 7.0. They ended up in the ER with internal bleeding.
The Institute for Safe Medication Practices says warfarin, insulin, and digoxin are the top three drugs involved in serious interaction-related emergencies. Together, they account for one-third of all interaction-related ER visits.
How to Protect Yourself
You don’t need to be a scientist to avoid these problems. Here’s what actually works:
- Keep a full list of everything you take. Not just prescriptions. Include over-the-counter meds, vitamins, herbal supplements, and even occasional painkillers. A 2020 study found patients who kept a written list reduced interaction risks by 47%.
- Use one pharmacy. Pharmacists can spot problems your doctor might miss. In the U.S., single-pharmacy use prevents about 150,000 adverse events every year.
- Ask specific questions. Don’t just say, “Is this safe?” Ask: “Could this interact with my other meds?” or “Are there foods I need to avoid?” Mayo Clinic research shows this increases detection of risks by 63%.
- Avoid grapefruit juice if you’re on any prescription drug. It interacts with 85 different medications. If you’re not sure, check the label or ask your pharmacist.
- Space out tricky combinations. If you take thyroid medication and calcium or iron supplements, wait at least four hours between them. That’s enough time for absorption to happen without interference.
What Doctors and Pharmacists Are Doing
Healthcare systems aren’t ignoring this. Most electronic health records now warn doctors about major interactions-85% of the time, according to a 2022 study. But doctors often ignore these alerts because they get too many. They’re tired of being told about low-risk issues.
Pharmacists are stepping in. Medication therapy management programs, where pharmacists sit down with patients to review all their drugs, reduce adverse events by 22% in older adults. In the U.S., pharmacist-led reviews prevent 1.2 million serious interactions each year.
Tools like Lexicomp and Micromedex give doctors and pharmacists detailed info on how each interaction works-and what to do about it. You don’t need to know these tools, but your provider should.
The Future: Personalized Medicine
Genetics are starting to play a bigger role. Some people naturally break down drugs slower because of their genes. For example, about 7% of people of European descent are “poor metabolizers” of CYP2C19. That means clopidogrel (a blood thinner) won’t work well for them. Testing for these traits is becoming more common.
The FDA now includes pharmacogenomic info on 340 drug labels. That means your doctor might soon test your genes before prescribing certain drugs. Early data suggests this could cut interaction-related hospital stays by 30%.
Telehealth platforms now check for interactions during virtual visits. In 2023, 78% of major U.S. health systems added this feature. It’s not perfect, but it’s helping.
One thing hasn’t changed: your body is unique. Age, kidney function, liver health, and other conditions all change how drugs behave. That’s why the American Geriatrics Society warns that older adults are at higher risk-40% of adults over 65 have reduced kidney function. What’s safe for a 30-year-old might be dangerous for a 70-year-old.
Bottom line: don’t assume your meds are harmless just because they’re legal or sold over the counter. The real danger isn’t the drugs themselves. It’s the hidden ways they talk to each other inside your body.
Stay informed. Stay organized. And never be afraid to ask your pharmacist: ‘Could this hurt me?’
What’s the difference between pharmacokinetic and pharmacodynamic drug interactions?
Pharmacokinetic interactions are about how your body handles the drug-how it’s absorbed, distributed, broken down, or removed. Pharmacodynamic interactions are about what the drugs do to your body when they’re both present. For example, taking two drugs that both lower blood pressure might cause your pressure to drop too far. That’s pharmacodynamic. One drug changing how fast another gets into your blood? That’s pharmacokinetic.
Can over-the-counter drugs cause serious interactions?
Yes. Many people think OTC means safe, but that’s not true. St. John’s Wort, a common herbal supplement for mood, can make birth control pills fail or reduce the effect of antidepressants and transplant drugs. Ibuprofen can increase methotrexate toxicity. Even antacids can stop your thyroid medicine from working. Always check with your pharmacist before taking anything new.
Why is grapefruit juice so dangerous with medications?
Grapefruit juice blocks an enzyme in your gut called CYP3A4. This enzyme normally breaks down many drugs before they enter your bloodstream. When it’s blocked, more of the drug gets absorbed. That can lead to overdose-like effects. For example, with statins, it can cause muscle damage. With blood pressure drugs, it can cause dangerously low blood pressure. About 85 prescription drugs have this warning. If you’re on any medication, avoid grapefruit juice unless your doctor says it’s okay.
Should I stop taking a medication if I think it’s interacting with another?
Never stop a prescribed medication on your own. Some drugs, like blood pressure or seizure meds, can cause serious withdrawal effects. Instead, call your doctor or pharmacist. They can help you adjust doses, switch medications, or space out timing safely. The goal is to keep you safe-not to stop treatment unless it’s absolutely necessary.
Are natural supplements safe to take with my prescriptions?
Not necessarily. Supplements aren’t tested like prescription drugs. St. John’s Wort, garlic, ginkgo, and green tea extract can all interfere with medications. Garlic and ginkgo can increase bleeding risk with warfarin. Green tea can reduce the absorption of some antibiotics. Always tell your provider what supplements you’re taking-even if you think they’re harmless.
Can alcohol interact with my medications?
Yes. Alcohol can increase drowsiness with sedatives, raise blood pressure with certain antidepressants, and damage the liver when taken with acetaminophen. The old belief that metronidazole and alcohol cause severe reactions has been questioned in recent years, but alcohol still affects how your liver processes many drugs. If you drink regularly, talk to your doctor about how it might affect your meds.






14 Comments
Really helpful breakdown! I’ve been taking statins and always wondered why my doc told me to skip grapefruit. Now it makes sense. Thanks for explaining it so clearly 😊
Let’s be real-this article is a sanitized corporate pamphlet. The FDA doesn’t care about you. They approve drugs with 85 known CYP3A4 interactions because pharmaceutical lobbying ensures zero accountability. Your ‘safe’ meds are a slow poison, and your pharmacist? Paid to look the other way. Wake up.
I appreciate how thorough this is. I’ve been on warfarin for years and never realized how easily something like ibuprofen could throw off my INR. I’ll definitely start keeping a written list now.
Thank you for this. I’ve been struggling to manage my meds since my stroke, and this clarity helped me feel less overwhelmed. I’m going to take my list to the pharmacy tomorrow. Small steps, right? 🙏
This is an exemplary piece of patient education. The ADME framework is elegantly simplified without sacrificing scientific accuracy. I recommend this to all my patients over 65. The emphasis on pharmacist collaboration is particularly vital.
Ugh. Another ‘trust your pharmacist’ propaganda piece. Did you know the FDA approved 340 drugs with pharmacogenomic warnings… but 92% of primary care docs don’t even order genetic tests? This is performative safety. You’re being sold a false sense of security while Big Pharma profits from your ignorance.
GRAPEFRUIT = BAD. 🍊❌💊
St. John’s Wort = sneaky! 🌿🤯
Ask your pharmacist. They’re the real MVPs. 💪❤️
Why are we letting foreigners and herbal nonsense dictate our medicine? In America, we don’t need ‘St. John’s Wort’ or ‘grapefruit warnings’-we need real drugs, not hippie tea. This article is weak. Trust your doctor, not some blog.
Everyone’s missing the point. CYP3A4 inhibition isn’t even the biggest threat-it’s the P-glycoprotein transporter synergy with SSRIs and beta-blockers that’s silently killing people. You think grapefruit is bad? Try taking sertraline with verapamil. That’s how you end up in a coma. But no, let’s just tell people to ‘ask their pharmacist.’ Pathetic.
Great resource. I’m an immigrant from Vietnam and didn’t realize how much my traditional ginger tea could interfere with my blood thinner. I’ll stop it tonight. Thank you for making this accessible.
While I appreciate the effort, this article is fundamentally flawed in its framing. It assumes patients are passive recipients of care. In reality, most are overwhelmed, undereducated, and financially strained. A ‘written list’ won’t help someone working three jobs who can’t afford to miss a shift to visit a pharmacist. This is virtue signaling disguised as patient advocacy.
Every time I read something like this, I’m reminded: medicine isn’t just science-it’s storytelling. You’ve given people a map to navigate a system that’s designed to confuse them. That’s powerful. Keep sharing this kind of clarity. We need more of it.
Bro, CYP2D6 poor metabolizers are everywhere in India-like 20% of us. I’ve seen patients on antidepressants crash because their doc didn’t know. Also, turmeric = CYP3A4 inhibitor. Don’t take it with statins. Trust me, I’ve seen the labs.
Simple truth: if you’re on more than 3 meds, you’re playing Russian roulette. Grapefruit? Avoid. Herbs? Avoid. Ask questions? Only if you have time. The system’s broken. End of story.