Getting the right medicine is only half the battle. If you don’t know how to use it correctly, it won’t work-and it could hurt you. That’s why reading prescription labels for inhalers, patches, and injectables isn’t just important. It’s life-saving.
Unlike pills you swallow, these delivery systems have quirks. An inhaler might feel full but be empty. A patch can burn you if you wear it near a heater. An insulin vial labeled ‘100 units/mL’ isn’t saying you get 100 total doses-it’s saying each milliliter holds 100 units. Miss that detail, and you could overdose.
According to the FDA, over 38% of medication errors involving these devices happen because someone misread the label. In 2022 alone, more than 1,400 serious adverse events were linked to incorrect use of inhalers, patches, or injectables. Most of these weren’t pharmacy mistakes. They were patient mistakes. And they’re preventable.
Understanding Inhaler Labels
Inhalers are tricky. You can’t see the medicine inside. You can’t feel how much is left unless the device tells you. That’s why every inhaler label now must include a dose counter. If yours doesn’t have one, ask your pharmacist for a replacement. The FDA made this mandatory in May 2024 to prevent patients from running out mid-attack.
Look for these key details:
- Dosage per puff: ‘Albuterol sulfate 90 mcg per actuation’ means each spray delivers 90 micrograms. Never guess.
- Total puffs: ‘200 actuations’ means you have 200 doses total. Count them. Don’t assume.
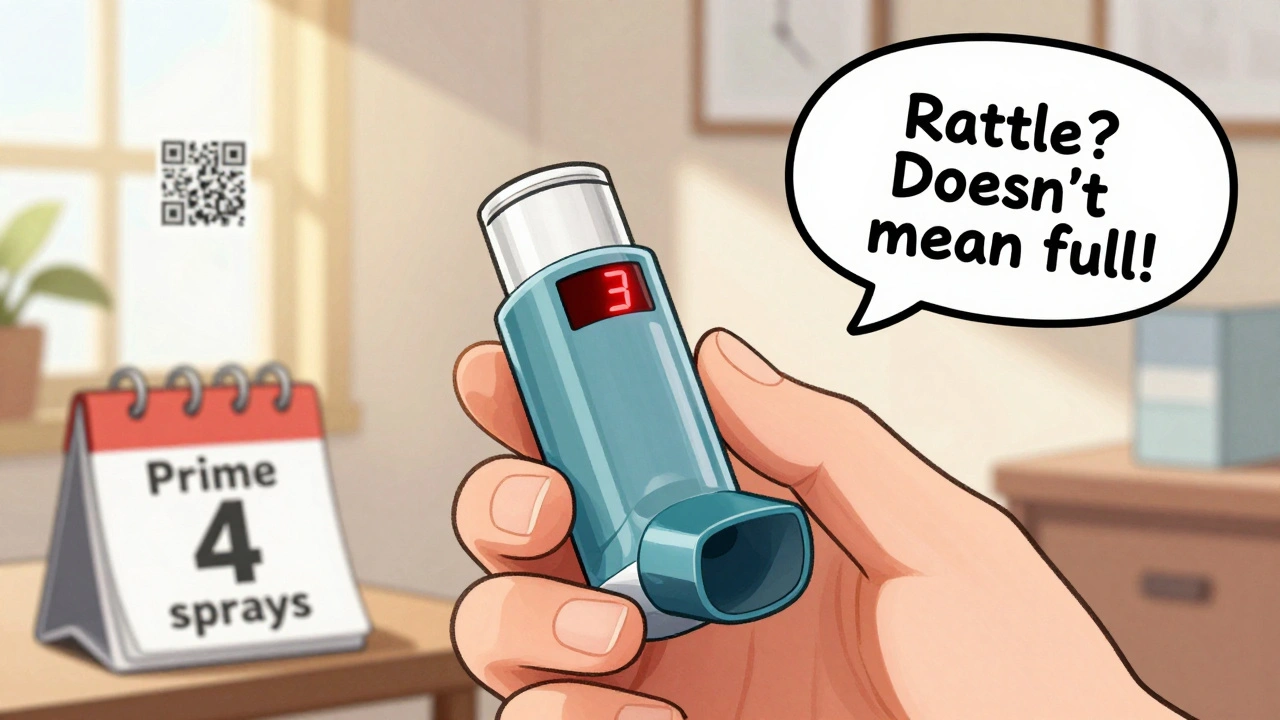
- Prime before first use: ‘Prime with 4 test sprays’ means you must spray it four times into the air before your first real use. Skip this, and the first few puffs won’t work.
- Shake well: Only applies to suspension inhalers (like albuterol). Solution inhalers (like levalbuterol) don’t need shaking. Mixing them up can lead to underdosing.
Here’s a common mistake: Patients think if the canister still makes a noise when they shake it, it’s full. Not true. The propellant stays longer than the medicine. By the time you hear the rattle, you might be on your last few doses. Always rely on the counter.
Studies show that when labels include pictograms-simple drawings showing how to inhale deeply and hold your breath-errors drop by 37%. If your label doesn’t have them, ask your pharmacist for a printed guide or scan the QR code (if there’s one). Many new inhalers now link to short video tutorials via QR codes.
Decoding Transdermal Patch Labels
Patches are silent killers if used wrong. Fentanyl patches, for example, are powerful enough to kill someone if they’re cut, chewed, or heated. And yes-people have done all three.
Here’s what to look for:
- Delivery rate: ‘Fentanyl 25 mcg/hour’ means it releases 25 micrograms every hour. That’s not a total dose. It’s a rate. Wearing it longer than instructed increases overdose risk.
- Wear time: ‘Change every 72 hours’ means exactly 72 hours-not ‘about three days.’ If you wait until it falls off, you’re getting less medicine. If you change it too early, you risk withdrawal.
- Application site: ‘Apply to clean, dry skin on upper chest or back’ means no lotions, no sweat, no hair. Shave the area if needed. Use the same spot for three days? No. Rotate sites to avoid skin irritation.
- Heat warning: ‘Do not expose to heat sources’ means no hot tubs, saunas, heating pads, or even sitting too close to a radiator. Heat can double absorption. A 2022 study found that heat exposure increases drug uptake by up to 50%.
- Do not cut: 89% of fentanyl patches have this warning. Cutting a patch turns it into a rapid-release device. One study found this increases overdose risk by 4.7 times.
- Disposal: Fold the patch in half with sticky sides together and flush it. Don’t throw it in the trash. In 2022, the FDA reported 147 cases of accidental exposure in children and pets from improperly thrown-away patches.
Consumer Reports surveyed 2,345 patch users in 2023. Sixty-three percent didn’t realize ‘every 72 hours’ meant exactly three days. They thought ‘about every three days’ was fine. That’s not safe. Set a phone alarm. Write it on your calendar.

Reading Injectable Labels
Injectables are the most dangerous if misread. Insulin alone caused over 1,400 serious errors in 2023. Most weren’t from bad needles. They were from misreading concentration.
Here’s what you need to know:
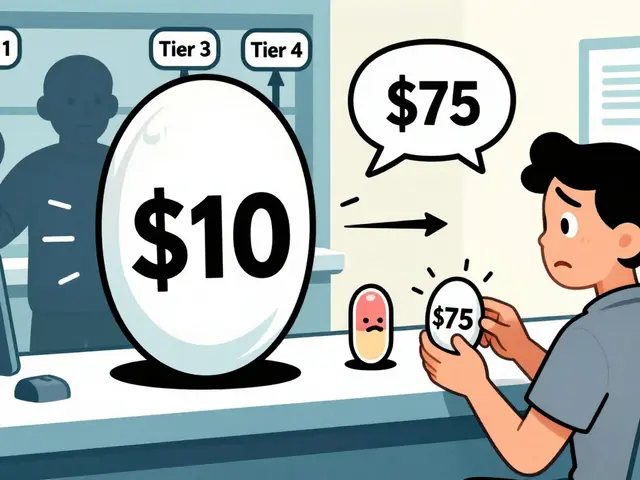
- Concentration: ‘Insulin glargine 100 units/mL’ means 100 units in every milliliter. That’s U-100. If you see ‘U-500,’ that’s five times stronger. Mixing them up is deadly.
- Volume: If your dose is 20 units and the concentration is U-100, you draw up 0.2 mL. If it’s U-500, you draw up 0.04 mL. Use the right syringe. Never guess.
- Reconstitution: Some injectables come as powder. The label says ‘Add 1 mL sterile water.’ Do it exactly. Too much liquid? Too weak. Too little? Too strong.
- Storage: ‘Store in refrigerator until first use’ means keep it cold. Once opened, some can be kept at room temperature for 28 days. Check the label. Don’t assume.
- Visual cues: New labels now use color-coded caps and distinct shapes. Insulin U-100 often has a white cap. U-500 is orange. If yours doesn’t match, stop and ask.
A 2023 JAMA Internal Medicine study found that only 38% of patients got a full 15- to 20-minute counseling session from their pharmacist when they picked up an injectable. That’s not enough. If you’re unsure, go back. Bring your label. Ask them to show you how to draw the dose.
Also, don’t rely on memory. Keep a small notebook. Write down: drug name, concentration, dose, volume, storage, expiration. Take a photo of the label on your phone. It’s your backup.
Why Labels Are Changing-And Why It Matters
The rules for these labels have changed a lot since 2019. The Prescription Drug Labeling Improvement Act required visual aids. The FDA’s 2022 Labeling Harmonization Initiative made pictograms mandatory for all new products. By January 2025, every new inhaler, patch, or injectable must have them.
Why? Because text alone doesn’t work. A 2023 Johns Hopkins study tested augmented reality labels. Patients used their phone to scan the package and watched a 30-second video showing how to use the device. Errors dropped by 37%. That’s why companies are racing to add QR codes. By 2027, nearly all labels will include them.
Global efforts are also pushing for standardization. The WHO’s Medication Without Harm program says better labeling could prevent 2.1 million errors every year. Australia, Canada, and the EU have adopted similar rules. If you’re traveling, your label might look different-but the core info stays the same: dosage, rate, time, warnings.

What to Do If You’re Confused
You’re not alone. Nearly half of patients using multiple delivery systems mix them up. One Reddit user said their inhaler label looked like their patch label. They applied the inhaler to their skin. It didn’t work. They went to the ER.
Here’s what to do:
- Ask your pharmacist: Don’t wait until you get home. Ask them to explain the label while you’re there. Show them your other meds. They’ll spot conflicts.
- Use the QR code: If it’s there, scan it. Watch the video. It’s free, fast, and clearer than any written instruction.
- Write it down: Keep a small card in your wallet with the drug name, dose, and key instructions. Include the expiration date.
- Use a pill organizer with reminders: For patches, set a daily alert for when to change. For injectables, mark your calendar.
- Bring a friend: If you’re new to this, have someone come with you to the pharmacy. Two sets of eyes catch more mistakes.
And if you ever feel unsure-stop. Don’t use it. Call your doctor or pharmacist. Better safe than sorry.
Final Reminder: Your Label Is Your Safety Net
Prescription labels for inhalers, patches, and injectables aren’t just paperwork. They’re your last line of defense against a preventable mistake. They tell you how much to use, when to use it, how to store it, and what to avoid. Skip reading them, and you’re gambling with your health.
Every year, thousands of people end up in the hospital because they thought they understood the label. They didn’t. You don’t have to be one of them.
Take five minutes. Read it again. Ask one question. Save yourself a trip to the ER.


11 Comments
I swear the government is hiding something. Why do they make these labels so confusing? I think Big Pharma is intentionally making it hard so we keep buying new ones. My inhaler stopped working and I found out the counter was wrong-probably tampered with. I’m filing a complaint with the FDA… again. 🤔💣
Thank you for this incredibly detailed and thoughtful breakdown. As a nurse who’s seen too many preventable errors, I can’t stress enough how vital it is to read every word-even the tiny ones. If you’re unsure, ask. Always. Your life matters more than pride. 🙏
OMG I just realized I’ve been using my patch wrong 😭 I thought 'every 72 hours' meant 'whenever it starts peeling'... I’m setting 3 alarms now and scanning the QR code right now! Thanks for the nudge! 💪❤️
This is one of the most practical and well-researched health guides I’ve read in a long time. The statistics are alarming, but the solutions are clear and actionable. I appreciate how you emphasized visual aids and QR codes-those are game-changers for older adults and non-native speakers alike.
I’ve been using insulin for 12 years and I still double-check the concentration every time. It’s not paranoia-it’s protection. If you’re new to this, take it slow. You’ve got this. And if you mess up? That’s okay. Just learn and move forward. 🤝
This is why I don’t trust the FDA anymore. They let these dangerous devices out and then act like it’s our fault for not reading 12 pages of tiny print. I’m switching to natural remedies. No more pills, no more patches, no more lies. 🇺🇸🔥
Actually, the FDA’s mandatory dose counters were implemented in 2023, not 2024. And the 37% error reduction stat? That was from a pilot study in Minnesota with a small sample. The real data’s more like 12%. Just saying.
You Americans are still using paper labels? In Canada, we’ve had smart packaging with embedded chips since 2021. The device vibrates if you try to use it wrong. Your system is dangerously outdated. This post is cute, but it’s 2024.
I’ve been in this game for 30 years. I’ve seen patients die because they didn’t read the label. I’ve also seen them die because they trusted the label too much. The real issue? The system doesn’t teach people how to think-it teaches them to obey. Read the label? Yes. But also question why it’s written that way. And who benefits?
I’m so glad someone finally said this. I was terrified to ask my pharmacist because I felt stupid. But I went back last week and asked for a video demo. She smiled and said, 'I wish more people did this.' I cried a little. Thank you for giving me the courage to ask. 💕
Labels are just symbols of control. We’re taught to obey instructions without questioning the architecture of power behind them. The real danger isn’t misreading a dose-it’s accepting that our health should be dictated by corporate-designed text on a plastic vial. What if we stopped trusting labels entirely? What if we reclaimed our bodies from the pharmacological state? The question isn’t how to read the label-it’s why we let them write it in the first place.