
More than 4 in 10 adults over 65 take five or more prescription drugs every day. For many, that’s not a choice-it’s a necessity. Heart disease, diabetes, arthritis, high blood pressure, and depression often come together, each needing its own medication. But when you’re taking 10 pills a day, the risk of dangerous drug interactions goes up fast. It’s not just about mixing pills. It’s about how your body reacts, how your organs handle the load, and whether you even still need all of them.
What Is Polypharmacy-and Why Does It Matter?
Polypharmacy isn’t just having a lot of medications. It’s taking five or more at the same time regularly. That’s the threshold where the chance of harmful side effects, hospital visits, or even death rises sharply. The World Health Organization calls it one of the biggest patient safety issues today. But not all polypharmacy is bad. If every pill has a clear reason, works as intended, and you can take it safely, then it’s appropriate. The problem comes when medications are added without a plan, forgotten about, or used to treat side effects from other drugs.
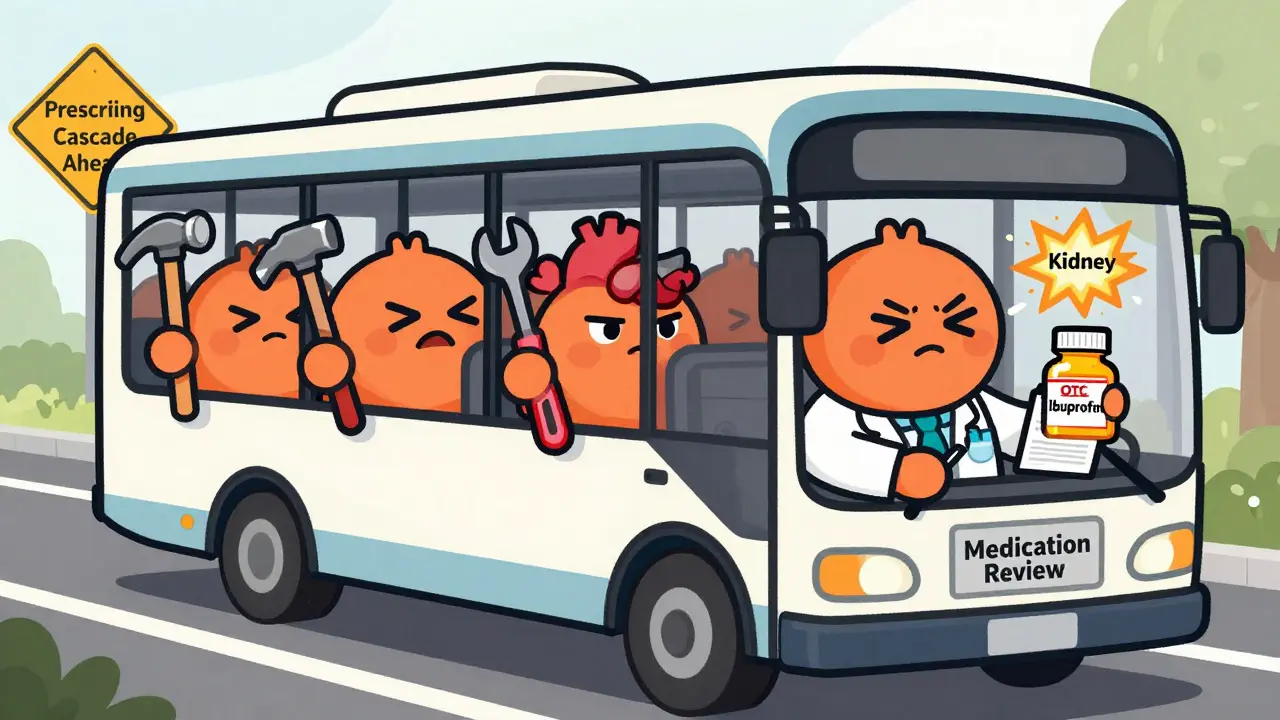
Think of it like this: You’re on a bus with 10 people, and each person is holding a different tool. One has a hammer, another a screwdriver, another a wrench. If they all start using their tools at once, something’s going to break. That’s what happens in your body. One drug lowers your blood pressure. Another makes you dizzy. So your doctor prescribes a third drug to stop the dizziness. Now you’re on three drugs for what started as one problem. That’s a prescribing cascade-and it’s common.
How Do Dangerous Drug Interactions Happen?
Drug interactions don’t always show up right away. Sometimes, they build slowly. Here’s how they usually happen:
- Multiple doctors, no coordination. You see a cardiologist, a rheumatologist, a neurologist, and your GP. Each writes prescriptions without knowing what the others prescribed. A painkiller from one doctor might raise your blood pressure, but your heart doctor doesn’t know you’re taking it.
- Over-the-counter meds and supplements. People don’t think of aspirin, ibuprofen, or fish oil as “medications.” But they can interfere with blood thinners, kidney function, or blood sugar control. A 2023 study found nearly 60% of older adults on multiple prescriptions also took at least one supplement without telling their doctor.
- Old meds that don’t fit anymore. You took a medication for a past infection, a temporary condition, or even a symptom that’s now gone. But no one ever stopped it. It’s just sitting there, adding to the pile.
- Slowed metabolism. As we age, our liver and kidneys don’t process drugs as quickly. That means even normal doses can build up to toxic levels over time.
Some of the most dangerous combinations involve blood thinners like warfarin, diabetes drugs like insulin, and heart medications like beta-blockers. Mixing these with common pain relievers or herbal supplements can lead to internal bleeding, dangerously low blood sugar, or sudden drops in heart rate.
The Five-Step Safety Plan for Managing Multiple Medications
Managing polypharmacy isn’t about cutting pills. It’s about making smarter choices. The World Health Organization and major medical groups agree on a clear five-step approach:
- Review every medication. Don’t just look at prescriptions. Bring everything-vitamins, herbal teas, sleep aids, cough syrups. Write down the name, dose, why you take it, and who prescribed it. If you can’t remember, take your pill organizer to your appointment.
- Ask: Is this still needed? For every drug, ask your doctor: “What is this for? Is it still helping? Could it be causing side effects?” If a medication was started years ago for a condition that’s now under control, it might be safe to stop.
- Look for prescribing cascades. If you’re taking a drug to fix a side effect of another drug, that’s a red flag. For example, if you’re on a diuretic that causes low potassium, and now you’re taking a potassium pill, that’s expected. But if you’re taking a stomach pill for nausea caused by a painkiller, maybe the painkiller should be changed instead.
- Use the fewest pills possible. Ask if any drugs can be combined into one pill. Ask if you can switch to a once-daily version. Simpler regimens mean fewer mistakes and better adherence.
- Deprescribe intentionally. Stopping a drug isn’t always easy. Some medications, like antidepressants or blood pressure pills, need to be tapered slowly. Stopping suddenly can cause rebound effects-your blood pressure spikes, your anxiety returns, or your heart races. Never stop a drug without your doctor’s guidance.
Deprescribing: When Less Is More
Deprescribing isn’t about taking fewer pills for the sake of it. It’s about removing drugs that no longer serve you. A 2024 review of clinical guidelines found that the most effective way to reduce harm from polypharmacy is through patient-centered medication reviews-where you and your doctor look at each pill together and decide what stays and what goes.
For example, an 80-year-old with mild dementia and high blood pressure might be on eight medications. One is for osteoporosis, but they haven’t had a bone density scan in five years. Another is a sleeping pill that makes them fall at night. A third is an old antibiotic that was prescribed for a urinary infection three years ago. After a review, three of those eight drugs were stopped safely. Their balance improved, their confusion lessened, and their risk of falls dropped by 40%.
Deprescribing works best when it’s slow and monitored. Your doctor might reduce a dose by 25% every two weeks. They’ll watch for symptoms. If you feel worse, they’ll pause. If you feel better, they’ll keep going. The goal isn’t to cut pills-it’s to cut risk.
Your Role: How to Take Control
You’re not just a patient. You’re the most important person in your medication team. Here’s what you can do right now:
- Keep a master list. Write down every medication you take-name, dose, time of day, reason, and prescriber. Use a notebook, phone app, or printable form from your pharmacy. Update it every time something changes.
- Use one pharmacy. All your prescriptions should come from the same place. Pharmacists can spot interactions your doctor might miss. They’ll flag if you’re getting two drugs that shouldn’t be mixed.
- Bring your pills to appointments. Don’t just say you take “the blue pill.” Show the bottle. Pictures help, but the actual bottle tells the pharmacist the exact strength and manufacturer.
- Link pills to habits. Take your morning pills right after brushing your teeth. Put your evening pills next to your bedtime glass of water. Routines reduce forgetfulness.
- Speak up about side effects. If you feel dizzy, tired, confused, or have new stomach pain, don’t assume it’s “just aging.” Tell your doctor. It might be a drug reaction.
- Ask before you try anything new. Don’t start a supplement, herbal remedy, or over-the-counter medicine without checking with your pharmacist or doctor first. Even “natural” can be dangerous.

Teamwork Makes It Work
Managing polypharmacy isn’t just your job-or your doctor’s. It takes a team. Pharmacists are your first line of defense. Nurses help track your progress. Caregivers can remind you to take pills and notice changes in behavior. When all of you are on the same page, mistakes drop.
Best practices include:
- Pharmacists doing full medication reviews during annual check-ups.
- Doctors using tools like the Beers Criteria-a list of medications that are risky for older adults.
- Hospitals and clinics doing medication reconciliation every time you’re admitted or discharged.
- Caregivers being included in discussions about treatment goals.
One Perth-based clinic started a program where every patient on five or more medications got a free pharmacist consultation every six months. Within a year, 32% of patients had one or more drugs stopped safely. Hospital visits for drug-related problems dropped by 27%.
What to Do If You’re Overwhelmed
If you’re taking a lot of medications and feel lost, you’re not alone. Start here:
- Write down every pill, supplement, and OTC drug you take.
- Call your pharmacy and ask them to print your full medication list.
- Make an appointment with your GP-not a specialist. Ask for a “medication review.”
- Bring your list and your pill organizer.
- Ask: “Which of these are absolutely necessary? Which might be doing more harm than good?”
You don’t need to fix everything at once. One less pill this month is progress. One fewer interaction is a win.
Final Thought: Safety Isn’t About Quantity-It’s About Clarity
Having five medications isn’t dangerous. Having five medications with no clear purpose, no coordination, and no review is. The goal isn’t to take fewer drugs. It’s to take the right drugs, for the right reasons, in the safest way possible.
Medications save lives. But they can also harm you-if you don’t know why you’re taking them, or if no one’s checking if they’re still needed. Ask questions. Keep records. Speak up. Your health isn’t just about what’s in the bottle. It’s about what’s in your head-and who’s helping you think clearly.
What is considered polypharmacy?
Polypharmacy is defined as the regular use of five or more medications at the same time. This threshold is used because research shows the risk of harmful drug interactions, side effects, and hospitalizations increases significantly beyond this point, especially in older adults. It doesn’t mean all five are unnecessary-some are essential. The issue is whether each one is still needed, safe, and properly monitored.
Can over-the-counter drugs and supplements cause dangerous interactions?
Absolutely. Common OTC drugs like ibuprofen, aspirin, and antacids can interfere with blood thinners, blood pressure medications, and kidney function. Supplements like St. John’s Wort, ginkgo biloba, garlic, and fish oil can thin the blood, lower blood sugar, or affect liver enzymes that process other drugs. Many people don’t realize these are active medications. Always tell your doctor and pharmacist about everything you take-even if you think it’s “just a vitamin.”
Is it safe to stop a medication on my own if I feel better?
No. Stopping certain medications suddenly can cause serious problems. For example, stopping a blood pressure pill can cause a dangerous spike in pressure. Stopping an antidepressant too fast can trigger anxiety, dizziness, or even seizures. Even some sleep aids and pain relievers can cause rebound symptoms. Always talk to your doctor before stopping or changing any medication. They may need to taper the dose slowly to avoid withdrawal effects.
How often should I get a medication review?
If you’re taking five or more medications, you should have a full medication review at least once a year. More often if you’ve recently been hospitalized, changed doctors, started a new medication, or noticed new side effects. Some pharmacies and clinics offer free reviews every six months for high-risk patients. Ask your pharmacist or GP if they offer this service.
What tools can help me manage my medications?
Use a pill organizer with compartments for morning, afternoon, evening, and night. Keep a written or digital “Medication Master List” that includes the name, dose, reason, prescriber, and instructions (e.g., “take with food”). Apps like Medisafe or MyTherapy can send reminders. But the most powerful tool is bringing your actual pill bottles to every doctor visit-no summaries, no lists. Just the real bottles. That’s how pharmacists catch the most errors.
Can deprescribing improve my quality of life?
Yes, often dramatically. Many people on multiple medications report feeling more alert, less dizzy, sleeping better, and having fewer stomach issues after one or two unnecessary drugs are stopped. A 2023 study showed that patients who underwent structured deprescribing had fewer falls, less confusion, and higher satisfaction with their care. Removing drugs that no longer help can reduce side effects, lower costs, and simplify your daily routine-all without losing health benefits.
What should I ask my doctor during a medication review?
Ask these five questions: 1) What is this medication for? 2) Is it still working? 3) Could it be causing any side effects I’m having? 4) Is there a simpler or safer alternative? 5) Can we try stopping or reducing it? Write them down before your appointment. Don’t be afraid to say, “I’m worried about how many pills I’m taking.” Most doctors want to help-they just need you to start the conversation.
Managing multiple medications isn’t about memorizing a long list. It’s about staying curious, asking questions, and working with your team to keep things simple, safe, and effective. The goal isn’t to take fewer pills-it’s to take only the ones that truly matter.






10 Comments
This made me think about my mom. She’s on 12 pills and doesn’t even know why half of them are there. I’m taking her to her doctor next week with all the bottles. No more guessing.
Love this. It’s not about hoarding pills like they’re collectible coins. It’s about keeping your body from turning into a chemical soup. One less pill = one less chance to feel like a zombie at 3pm. 🙌
My grandma stopped her sleeping pill after her pharmacist said it was making her fall. She sleeps better now without it. Just shows you don’t always need more - sometimes you need less.
You’re not weak for needing meds. But you’re strong for asking if you still need them. Keep going. You got this.
My aunt took 8 meds. Now she takes 4. She’s walking again. Dancing at family weddings. Her doctor didn’t even know she was taking that old anxiety pill from 2012. She just forgot to stop it. We all need someone to say ‘wait, why are you still doing this?’
Oh wow. Another article telling us to ‘just ask your doctor’ like they have 47 hours to review your 12 meds. Meanwhile, your GP is on a 10-minute timer, juggling 30 patients, and you’re supposed to be the expert on pharmacokinetics? Cute. I’ll just keep my 11 pills and my silent suffering. 🤷♀️
Carol, you’re not wrong. The system’s broken. But here’s the thing - if you don’t start somewhere, nothing changes. Even if your doctor’s rushed, show up with your bottles. Say ‘I think one of these might be hurting me.’ That’s not asking for perfection. That’s asking for dignity. And that’s enough to start a conversation. I’ve seen it work. Even in 10 minutes. Even with a tired doctor. You just have to say it out loud.
It’s not about being a perfect patient. It’s about being a persistent one. Your body’s telling you something. Don’t let bureaucracy mute it.
I used to think meds were magic. Now I know they’re tools. And like any tool, if you don’t know why you’re holding it - you might cut yourself.
Deprescribing isn’t giving up. It’s choosing to live better, not just longer. And that’s worth fighting for.
Polypharmacy is a red herring. The real issue is poor clinical decision-making under resource constraints. The Beers Criteria are outdated and lack granularity for comorbid geriatric syndromes. You can’t deprescribe without a functional assessment, cognitive screening, and pharmacogenomic data - none of which are reimbursed. This article reads like a pamphlet from a pharma-adjacent advocacy group.
Is there data on how many people actually get a full med review? I’ve heard the stats - but what’s the real-world uptake? Like, is it under 10%?
Yeah. Under 15% in primary care. Even less in rural areas. But that’s why the pharmacy-based reviews are so important - they’re accessible, free, and not dependent on a doctor’s schedule. The Perth clinic example? That’s the model. Pharmacists are the unsung heroes here. They’re the ones who catch the double-dosing, the interactions, the ghosts of prescriptions past. If we want change, we need to fund and empower them - not just tell patients to ‘ask more’.