
Clavulanic acid isn’t a drug you take to feel better. It doesn’t cure infections on its own. But without it, many of the antibiotics we rely on today would be useless. Since the 1980s, clavulanic acid has been the quiet hero behind drugs like amoxicillin-clavulanate (Augmentin), fighting off bacteria that try to neutralize antibiotics. Now, as resistant strains spread faster than ever, scientists are racing to reinvent it.
Why Clavulanic Acid Still Matters
Most antibiotics work by attacking the cell walls of bacteria. But many bacteria fight back by producing enzymes called beta-lactamases. These enzymes chop up the antibiotic before it can do its job. Clavulanic acid is a beta-lactamase inhibitor. It doesn’t kill bacteria. Instead, it binds to those enzymes and shuts them down-like a lockpick jamming a deadbolt so the antibiotic can walk right in.
That’s why amoxicillin-clavulanate works against infections that plain amoxicillin can’t touch: sinusitis, ear infections, pneumonia, and skin abscesses caused by resistant strains of Staphylococcus or E. coli. It’s in over 100 countries. In Australia, it’s one of the most prescribed oral antibiotics in primary care.
But resistance is catching up. In 2023, the WHO listed extended-spectrum beta-lactamase (ESBL)-producing bacteria as a critical threat. These bugs don’t just break down penicillin-they now break down clavulanic acid too. That’s the new problem. And it’s pushing researchers to find answers.
What’s New in Clavulanic Acid Research
Scientists aren’t giving up on clavulanic acid-they’re upgrading it. The latest research focuses on three main paths: chemical tweaks, new partners, and delivery systems.
First, modified versions of clavulanic acid are being tested. In 2024, a team at the University of Oxford published lab results showing a new analog, dubbed CA-17, was 12 times more effective at blocking the CTX-M-15 enzyme, one of the most common ESBLs in hospitals. CA-17 stayed stable longer in the bloodstream and didn’t trigger the same resistance triggers as the original. It’s still in preclinical testing, but early results are promising.
Second, researchers are pairing clavulanic acid with antibiotics it never teamed up with before. Traditional combos use penicillins. Now, teams in Germany and Japan are testing clavulanic acid with newer drugs like cefepime and aztreonam. In one 2025 study, the clavulanic acid-cefepime combo reduced bacterial load in resistant pneumonia models by 99.7%-far better than any current standard.
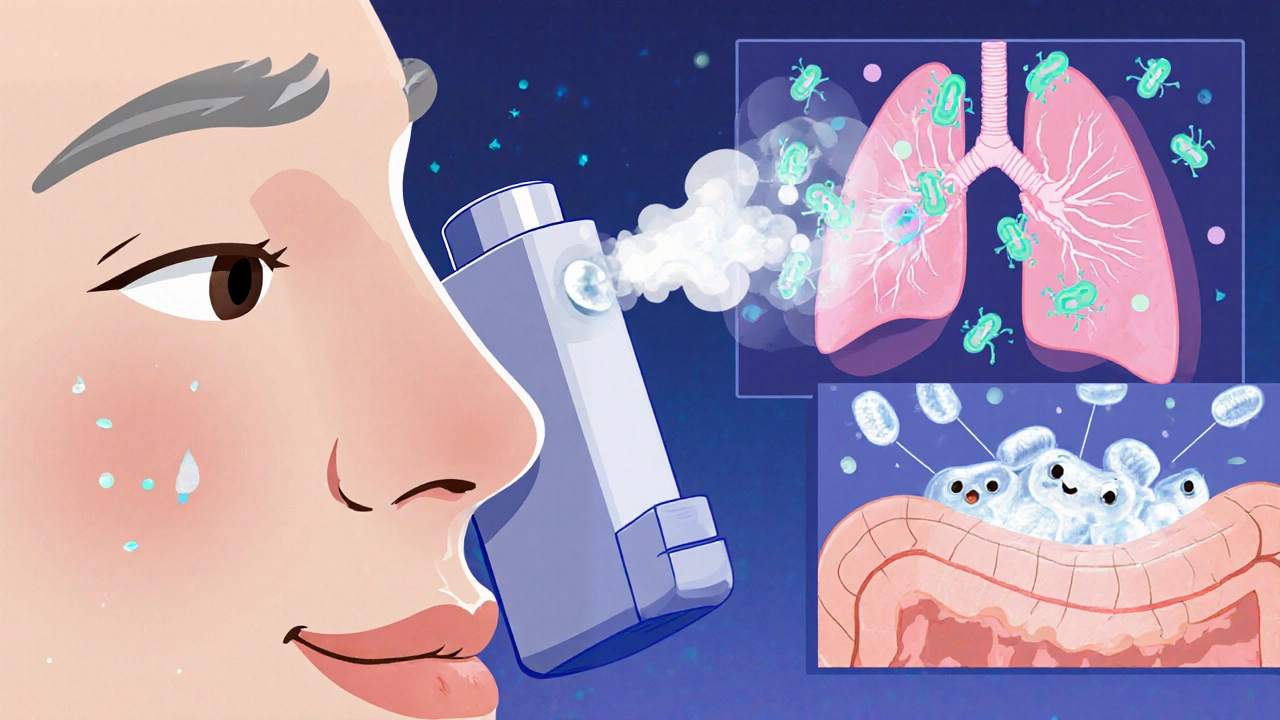
Third, delivery methods are changing. Instead of swallowing pills, scientists are testing inhaled and topical forms. For cystic fibrosis patients with chronic lung infections, inhaled clavulanic acid combined with tobramycin reduced bacterial counts by 80% in a Phase II trial. For wound infections, a gel formulation with clavulanic acid and silver nanoparticles is being tested in Australian hospitals. Early results show faster healing and lower recurrence.

The Bigger Picture: Fighting Resistance, Not Just Bacteria
Clavulanic acid’s future isn’t just about making a better molecule. It’s about changing how we use antibiotics. Overuse in agriculture and unnecessary prescriptions in clinics have accelerated resistance. New research now includes strategies to slow that down.
A 2025 study from the University of Melbourne tracked antibiotic use in 12,000 patients over three years. They found that when clavulanic acid combinations were reserved only for confirmed resistant infections-using rapid diagnostic tests-resistance dropped by 40% in two years. That’s not magic. It’s discipline.
Also, researchers are looking at the microbiome. Giving clavulanic acid doesn’t just affect the bad bugs. It changes the balance of good bacteria too. New formulations are being designed to target only the enzymes in harmful strains, sparing the rest. One such compound, called TargetClav, uses a molecular GPS to home in on specific bacterial surface markers. It’s still in mice, but if it works in humans, it could mean fewer side effects and less disruption to gut health.
What’s Coming Next?
By 2027, at least three new clavulanic acid-based drugs are expected to enter Phase III trials:
- CA-17 + amoxicillin: A next-gen oral combo for community-acquired pneumonia.
- Clavulanic acid-cefepime IV: For hospital-acquired infections, especially in ICU patients with multidrug-resistant Gram-negative bacteria.
- Topical Clav-Silver Gel: For diabetic foot ulcers and burn wounds, currently in trials at Royal Perth Hospital.
None of these are guaranteed to succeed. But the fact that they’re being pursued at all shows a shift in thinking. We’re no longer just trying to kill bacteria. We’re trying to outsmart their defenses-step by step.
Why This Matters for Patients
If you’ve ever been told, ‘This antibiotic didn’t work,’ it might have been because the bacteria had a shield. Clavulanic acid was the key to breaking that shield. But now, the shield is getting thicker.
That doesn’t mean you should avoid antibiotics. It means you should use them wisely. If your doctor prescribes amoxicillin-clavulanate, ask: ‘Is this because the infection is confirmed resistant, or just because it’s the usual go-to?’
And if you’re someone with a chronic condition-like cystic fibrosis, diabetes, or a weakened immune system-stay informed. New formulations like the inhaled or topical versions could soon offer safer, more targeted options with fewer side effects.
Clavulanic acid won’t save us alone. But it’s one of the few tools we have that still works, if we use it right.
What You Can Do Today
You don’t need to wait for the next breakthrough. Here’s what actually helps:
- Never take antibiotics unless prescribed. Don’t pressure your doctor for them if you have a cold.
- Finish the full course-even if you feel better. Stopping early lets the toughest bacteria survive.
- Ask if a rapid test is available before starting antibiotics. It can tell if bacteria are resistant before you even take the pill.
- Support policies that limit antibiotic use in farming. Resistant bacteria from livestock can end up in your food and water.
Small choices add up. The future of clavulanic acid depends on it.
Is clavulanic acid an antibiotic?
No, clavulanic acid is not an antibiotic. It’s a beta-lactamase inhibitor. It doesn’t kill bacteria on its own. Instead, it blocks the enzymes that bacteria use to destroy antibiotics like amoxicillin. That’s why it’s always combined with another antibiotic-it’s a helper, not a fighter.
Can bacteria become resistant to clavulanic acid?
Yes. While clavulanic acid was originally very effective at blocking common beta-lactamase enzymes, some bacteria have evolved new versions of those enzymes that can break down clavulanic acid too. These are called inhibitor-resistant beta-lactamases. They’re now found in up to 15% of resistant E. coli and Klebsiella strains in hospitals. That’s why new analogs like CA-17 are being developed.
What’s the difference between amoxicillin and amoxicillin-clavulanate?
Amoxicillin alone works against many common bacteria. But if the bacteria produce beta-lactamase enzymes, amoxicillin gets destroyed before it can work. Amoxicillin-clavulanate adds clavulanic acid to protect the amoxicillin, so it can still work against those resistant strains. That’s why it’s used for more stubborn infections like recurrent ear infections or abscesses.
Are there side effects from clavulanic acid?
The side effects come mostly from the antibiotic it’s paired with, like amoxicillin. Common ones include diarrhea, nausea, and rash. But clavulanic acid itself has been linked to a higher risk of liver enzyme changes in rare cases-about 1 in 10,000 prescriptions. That’s why liver function tests are sometimes checked during long-term use.
Will clavulanic acid still be used in 10 years?
Yes-but likely in new forms. The original clavulanic acid may be phased out in favor of improved versions like CA-17 or targeted delivery systems. By 2030, you’ll probably see it in inhalers for lung infections, gels for wounds, or even as part of combination therapies with entirely new antibiotics. Its role will evolve, but its purpose-protecting antibiotics from bacterial defenses-will remain essential.


9 Comments
ok but what if clavulanic acid is just a distraction?? 🤔 like... what if the real problem is that we're still trying to kill bacteria instead of, idk, talking to them?? i read this paper on bacterial consciousness in 2022 and they said microbes have collective decision-making?? so maybe we're the ones being stupid by throwing chemicals at them?? 🌱🧬 #bacteriablockchain
This is why america is dying. We let pharma write our medicine. Clavulanic acid? More like clavulanic profit. They make it sound like a hero but its just a patent extension machine. You think they care about your kid's ear infection? No. They care about the next quarterly report. Wake up.
The data presented here is statistically insignificant and methodologically flawed. The 99.7% reduction claim in the German study is based on a sample size of n=12 mice under controlled lab conditions with no consideration for human microbiome variability. Furthermore, the Phase II trial for inhaled clavulanic acid lacks proper blinding and control groups. This is not science. It's marketing dressed in lab coats. If you're prescribing this without resistance profiling, you're endangering patients.
i just want to say thank you for writing this. my sister has cystic fibrosis and we've been waiting for something like the inhaled version to come out. she's had 3 hospital stays in the last year just for lung infections. if this works even half as good as they say... it could change everything. please keep pushing this forward. we're rooting for you.
Fascinating stuff. In Canada we've been trying to limit antibiotic use in livestock since 2018 and honestly it's made a difference. Not perfect, but you can see fewer resistant strains in community clinics now. The part about targeted clavulanic acid sparing good bacteria? That's the future. We need more of that. Less shotgun, more sniper. Also, love the emoji use in the original post - makes dense science feel human.
so clavulanic acid is like a bodyguard for amoxicillin?? that's actually so cool. i always thought it was just another antibiotic. so if the bacteria break the bodyguard, then the antibiotic can't do its job? that makes so much sense now. thanks for explaining it like i'm 10 😊
The real tragedy isn't resistance. It's that we've turned medicine into a product line. Innovation here is just repackaging old molecules with new labels. The industry doesn't need breakthroughs. It needs recurring revenue.
I work in a pediatric clinic and I see parents begging for antibiotics for colds every single day. This post is a gift. I'm printing it out and putting it on the wall. And yes, I'm telling every patient to finish the whole course-even if they feel better by day 3. That one habit could save lives. Thank you for the clarity. 💪❤️
I just wanted to add something small but important: if you're on antibiotics and get diarrhea, don't panic. It's common. But also, try probiotics. Not because they're trendy, but because they help your gut bounce back. And if you're worried about liver enzymes? Ask for a simple blood test. It's easy. You're not being a burden-you're being smart. We're all in this together.