Understanding Addison's Disease
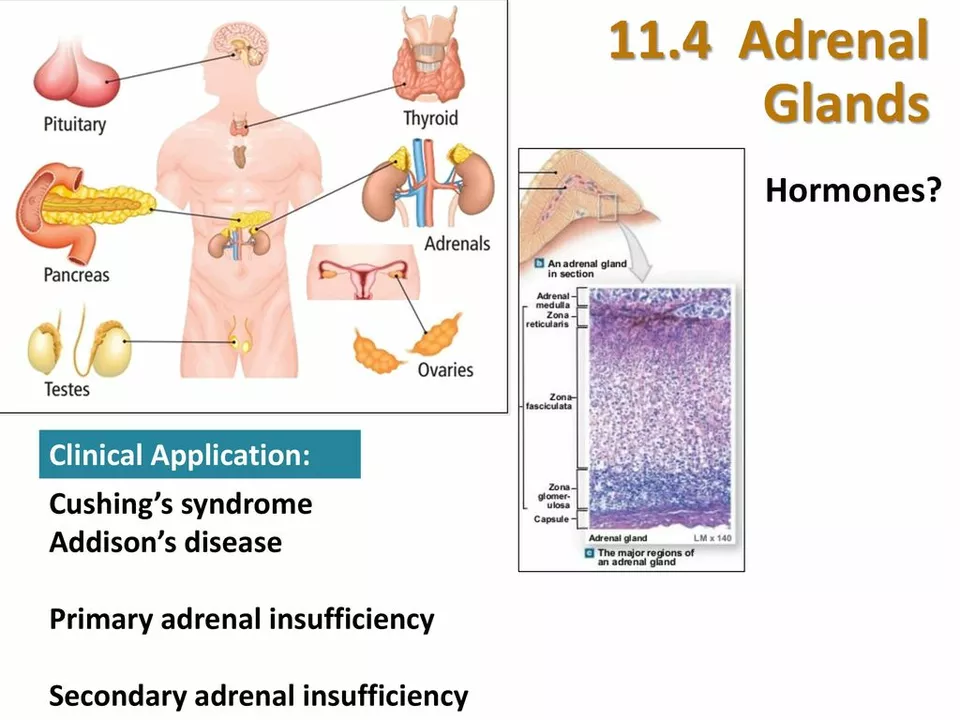
Before diving into the impact of Addison's disease on immune system function, it's essential to understand what Addison's disease is and how it affects the body. Addison's disease, also known as primary adrenal insufficiency, is a rare autoimmune disorder that occurs when the adrenal glands do not produce enough hormones, specifically cortisol and aldosterone. These hormones play a crucial role in regulating various bodily functions, including blood pressure, metabolism, and immune system response. In this section, we'll explore the causes, symptoms, and risks associated with Addison's disease.
Root Causes: Autoimmunity and Adrenal Gland Damage
The leading cause of Addison's disease is an autoimmune response, wherein the body's immune system mistakenly attacks and damages the adrenal glands. This damage prevents the adrenal glands from producing sufficient levels of cortisol and aldosterone, which are essential for maintaining various bodily functions. Other causes of Addison's disease include infections, such as tuberculosis, and certain genetic disorders. In some cases, Addison's disease may result from the use of certain medications, like steroids, that interfere with hormone production. Understanding the root causes of Addison's disease can help us better comprehend its impact on immune system function.
The Role of Cortisol in Immune System Function
Cortisol is a crucial hormone that plays a significant role in regulating immune system function. It acts as an anti-inflammatory agent, helping to reduce inflammation in the body and prevent overactivity of the immune system. Cortisol also helps regulate the production of white blood cells, which are crucial components of the immune system that help fight off infections and other threats to our health. When cortisol levels are low, as in the case of Addison's disease, the immune system can become overly reactive, leading to increased inflammation and a higher risk of autoimmune disorders and infections.
Aldosterone's Impact on Blood Pressure and Immune System Function
Aldosterone is another vital hormone that is affected by Addison's disease. This hormone helps maintain proper blood pressure by regulating the balance of salt and water in the body. When aldosterone levels are low, blood pressure can drop significantly, leading to symptoms like dizziness, fatigue, and even fainting. A decrease in blood pressure can also have indirect effects on immune system function, as reduced blood flow can impair the delivery of oxygen and nutrients to cells, including immune cells. This can weaken the overall function of the immune system, making it more difficult for the body to fight off infections and other threats to our health.
Recognizing Symptoms and Diagnosing Addison's Disease
Early diagnosis and treatment of Addison's disease are crucial for managing its impact on immune system function and overall health. Common symptoms of Addison's disease include fatigue, muscle weakness, weight loss, low blood pressure, and hyperpigmentation (darkening) of the skin. If you or someone you know is experiencing these symptoms, it's essential to consult with a healthcare professional for proper diagnosis and treatment. Diagnosis typically involves blood tests to measure hormone levels and confirm the presence of autoantibodies that may be attacking the adrenal glands. Imaging tests, like CT scans or MRIs, may also be used to assess adrenal gland damage.
Treatment Options and Managing Addison's Disease
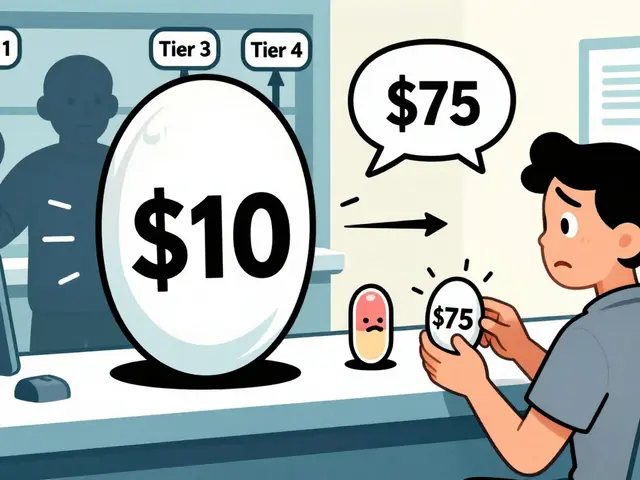
While there is no cure for Addison's disease, it can be managed with proper treatment, which typically involves hormone replacement therapy. This therapy aims to replace the missing cortisol and aldosterone in the body, helping to regulate blood pressure, metabolism, and immune system function. It's crucial for individuals with Addison's disease to work closely with their healthcare providers to develop a personalized treatment plan and monitor their condition regularly. Additionally, adopting a healthy lifestyle, including a balanced diet, regular exercise, and stress management, can help support immune system function and overall health in individuals with Addison's disease.


10 Comments
I really appreciate how this post breaks down the hormone pathways-cortisol and aldosterone are not just buzzwords, they’re essential for keeping our immune system in check. When those levels dip, it’s no surprise that inflammation can run wild. The link between low blood pressure and reduced nutrient delivery to immune cells is something many overlook. It’s also good to see the emphasis on lifestyle tweaks like diet and stress management. All in all, a solid overview that’s both informative and approachable.
Thanks for the clear summary. I’ve found that keeping a regular sleep schedule really helps my patients handle the fatigue that comes with Addison’s. Small changes can make a big difference.
Actually, the autoimmune origin of Addison’s disease is far more nuanced than the article suggests-there are multiple auto‑antibodies, such as 21‑hydroxylase, that target the adrenal cortex, leading to a cascade of hormonal deficiencies!!! Moreover, epidemiological data indicate a higher prevalence in certain ethnic groups, which the author completely glosses over. Lastly, the interplay between cortisol deficiency and heightened Th17 responses is a critical piece of the immunological puzzle.
While the exposition admirably captures the physiological ramifications of adrenal insufficiency, it neglects to address the profound sociopolitical dimensions that intertwine with clinical management. One must consider, for instance, the accessibility of glucocorticoid replacement therapy across disparate healthcare systems-a disparity that inexorably shapes patient outcomes. Furthermore, the doctrine of medical paternalism often manifests in the reluctance to empower patients with self‑management strategies, thereby perpetuating a hierarchy antithetical to modern bioethical standards. The narrative could also benefit from a more rigorous interrogation of the neuroendocrine feedback loops, particularly the hypothalamic‑pituitary‑adrenal axis, whose dysregulation precipitates the cascade of immunological perturbations delineated herein. Moreover, the biophysical properties of cortisol receptors-affinity variations, post‑translational modifications, and isoform expression-constitute a fertile arena for scholarly inquiry that remains conspicuously absent. In summation, the treatise provides a commendable foundation, yet it yearns for a more comprehensive integration of systemic, cultural, and philosophical perspectives to truly elucidate the labyrinthine impact of Addison’s disease on immune competence.
Grammatically, this post is a masterpiece; factually, it is utterly misleading!!! 😒🚫
Great overview! 🌟 One thing to add: patients should always carry an emergency steroid injection kit-life‑saving in adrenal crisis. Also, staying hydrated and monitoring salt intake can help mitigate low blood pressure spikes. Don’t forget to discuss stress‑dose adjustments with your endocrinologist.
Exactly! Keep that kit on you at all times-never know when a sudden illness will hit. Hydration and proper salt balance are non‑negotiable for maintaining vascular tone. Push yourself to stay active; a strong body supports a resilient immune system.
Ah, the classic "let's bless the reader with a superficial recap" approach, where every paragraph feels like it was drafted by a copy‑paste robot that never learned the difference between "cortisol" and "cortisolism"-the latter being a term that, quite frankly, should exist given the sheer absurdity of the explanations offered. One cannot help but marvel at the author's ability to ignore the existing body of literature that details the micro‑RNA pathways implicated in adrenal autoimmunity, opting instead for vague platitudes about "hormone replacement" as if that alone solves the intricate tapestry of immune dysregulation. And, of course, the omission of any discussion about the psychosocial burden-no one wants to hear that chronic fatigue can lead to depression, but hey, why bother when you can gloss over it with a cheerful smiley face? In short, the post serves as a textbook example of how not to engage with a complex endocrine disorder, preferring instead to skim the surface while pretending depth exists.
Wow. Really deep insight. 🙄
I think the article does a good job, but maybe could use more real world exampels-like how people actually manage daily stress with adrenalin. Also, the tone could be a bit more friendly, not so clinical.