
Antifungal & Antiviral Interaction Checker
Check Your Medication Combination
Select your antifungal or antiviral and H2 blocker to see if there's an interaction and how to take them safely.
When you're taking medication for an infection-whether it's a stubborn fungal rash or a viral illness like HIV-your stomach acid might be working against you. That’s because common heartburn drugs called H2 blockers can seriously interfere with how well antivirals and antifungals work. It’s not just a theoretical concern. Real patients have had treatment fail because their acid-reducing meds were taken at the wrong time-or not adjusted at all.
What Are H2 Blockers, Really?
H2 blockers, or histamine H2-receptor antagonists, are drugs that calm down stomach acid production. They’re not new-cimetidine (Tagamet) hit the market in 1977 and was the first of its kind. Today, you’ll mostly see famotidine (Pepcid), cimetidine, and nizatidine (Axid) on shelves. Ranitidine (Zantac) is gone, pulled from stores in 2020 after it was found to contain traces of a probable cancer-causing chemical called NDMA.These drugs work by blocking histamine from telling your stomach to make acid. Normal stomach pH is between 1 and 3-super acidic, like vinegar. H2 blockers raise that to 4-6, which sounds harmless until you realize that some life-saving drugs need that acidity to dissolve and get absorbed.
Why This Matters for Antifungals
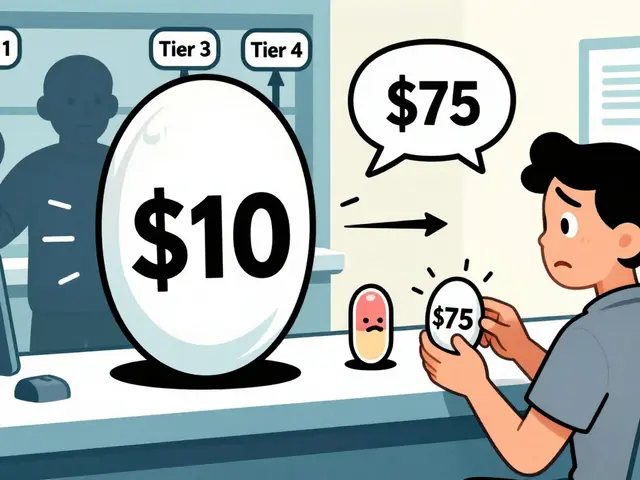
Not all antifungals are the same. Some need acid to work. Others don’t care at all. The difference can mean the difference between recovery and a worsening infection.Itraconazole, for example, is a powerful antifungal used for serious infections like aspergillosis or nail fungus. But it’s a diva when it comes to stomach pH. Studies show that when you take itraconazole with an H2 blocker, its absorption drops by 40-60%. That’s not a small dip-it’s enough to let the fungus grow unchecked. The tablet form is especially vulnerable. The oral solution? It’s formulated with citric acid and holds up better, even with acid suppression.
On the flip side, fluconazole doesn’t care. It dissolves easily in water, no matter how alkaline your stomach gets. You can take it with famotidine and still get full benefit. Same goes for voriconazole-it’s mostly unaffected by pH changes, but here’s the catch: it’s metabolized by liver enzymes that cimetidine can block.
That’s where things get complicated. Cimetidine doesn’t just change pH-it inhibits CYP450 enzymes, especially CYP2C19 and CYP3A4. These enzymes break down drugs like voriconazole. When cimetidine slows them down, voriconazole builds up in your blood. That can lead to toxicity: hallucinations, liver damage, or even heart rhythm problems. Famotidine? It doesn’t touch those enzymes. So if you need an H2 blocker and are on voriconazole, famotidine is the safer pick.
Isavuconazole (Cresemba) is the new kid on the block. It’s designed to cause fewer drug interactions. In clinical trials, it caused 26% fewer dose adjustments than voriconazole when used with other meds. That’s a big deal for patients on multiple drugs.
Antivirals and the Acid Problem
Antivirals aren’t off the hook either. Take atazanavir, an HIV protease inhibitor. It needs acid to dissolve properly. When taken with famotidine, its absorption can drop by up to 77%. That’s not just a warning on a label-it’s a real risk of the virus rebounding, leading to drug resistance.The FDA reviewed 42 antiviral labels in 2022. Nearly 7 out of 10 had specific warnings about acid-reducing drugs. But here’s the scary part: 31% of those antivirals didn’t even say *how* to take them safely. No timing. No instructions. Just a vague note. That’s a recipe for mistakes.
Other antivirals like dasatinib (used for certain leukemias and sometimes off-label for viral conditions) also rely on stomach acid. Even ketoconazole (an older antifungal still used in some cases) can’t be absorbed properly if your stomach pH is too high.
Cimetidine vs. Famotidine: The Real Difference
Not all H2 blockers are created equal. Cimetidine is the troublemaker. It’s the only one with an imidazole ring-that’s the chemical structure that lets it jam up liver enzymes. As a result, it interacts with over 40 drugs. Famotidine? It doesn’t do that. It’s clean. It only affects pH.Here’s what that means in practice:
- If you’re on itraconazole or atazanavir → avoid cimetidine. Use famotidine instead.
- If you’re on voriconazole → famotidine is safer, but still separate doses by 2 hours.
- If you’re on fluconazole → you’re mostly fine with any H2 blocker, but timing still matters for consistency.
According to the University of Liverpool’s drug interaction database, cimetidine accounts for 63% of all documented interactions with antifungals and antivirals. Famotidine? Only 12%. That’s not even close.
How to Take Them Safely
Knowing the problem isn’t enough. You need to know what to do.For pH-dependent drugs (itraconazole, atazanavir, ketoconazole):
- Take the antiviral or antifungal at least 2 hours before the H2 blocker.
- Use the oral solution of itraconazole if available-it’s more reliable.
- Never take them together unless instructed by a pharmacist or doctor.
For enzyme-inhibiting risks (voriconazole + cimetidine):
- Avoid cimetidine entirely.
- If you must use an H2 blocker, pick famotidine.
- Get your voriconazole blood levels checked after two weeks-target range is 2-5 mcg/mL.
Even with the best advice, mistakes happen. A 2022 survey of 1,200 hospital pharmacists found only 43% consistently told patients how to time their meds. That’s a huge gap. Patients assume if both are pills, they can swallow them together. They shouldn’t.

Why H2 Blockers Might Be Better Than PPIs
You might wonder-why not just switch to a proton pump inhibitor (PPI) like omeprazole? It’s stronger, right?Actually, no. PPIs suppress acid for over 24 hours. H2 blockers last only 6-12 hours. That means if you take famotidine at night, your stomach acid comes back by morning. You can take your antifungal in the morning on an empty stomach, when acid levels are higher, and avoid the interaction entirely.
ASHP guidelines actually recommend H2 blockers over PPIs when you need acid suppression alongside antifungals. Why? Because you have more control. You can time it. With PPIs, you’re stuck with low acid all day.
What’s Changing in the Future
The FDA is pushing for change. In late 2023, they proposed new labeling rules requiring all pH-sensitive drugs to include specific timing instructions. That could cut interaction-related failures by 35%.Researchers are also testing new formulations of itraconazole that don’t rely on stomach acid-like lipid-based carriers that deliver the drug directly into the bloodstream. Early trials (NCT04821542) are promising. If they work, we might finally be able to take these drugs without worrying about heartburn meds.
For now, though, the rules are simple: know your drugs. Know your stomach. And never assume two pills can be taken together.
Can I take famotidine with fluconazole?
Yes, you can. Fluconazole doesn’t need stomach acid to be absorbed, and it doesn’t interact significantly with famotidine. You can take them together without worrying about reduced effectiveness or toxicity.
Is cimetidine safe to use with antivirals?
No, it’s not recommended. Cimetidine blocks liver enzymes that break down many antivirals, including atazanavir and some HIV drugs. This can cause dangerous buildup of the antiviral in your blood, leading to side effects like nausea, liver damage, or heart rhythm issues. Always choose famotidine instead if you need an H2 blocker.
Why does itraconazole fail when taken with H2 blockers?
Itraconazole needs a low pH (acidic environment) to dissolve properly in your stomach. H2 blockers raise your stomach pH to 4-6, which prevents the drug from dissolving. As a result, your body absorbs 40-60% less of the drug, making it ineffective against the infection.
How long should I wait between taking an antiviral and an H2 blocker?
Wait at least 2 hours. Take the antiviral first, on an empty stomach, when your stomach acid is highest. Then take the H2 blocker later. This gives the antiviral time to absorb before acid levels drop.
Are there alternatives to H2 blockers for heartburn if I’m on antifungals?
Yes. Lifestyle changes like avoiding spicy foods, eating smaller meals, and not lying down after eating can help. For medication, antacids like Tums or Maalox can be used occasionally-they neutralize acid right away but don’t last long. If you need daily relief, famotidine taken 2 hours after your antifungal is still the safest option.
Can I take H2 blockers with isavuconazole?
Yes, and it’s one of the safest combinations. Isavuconazole (Cresemba) has minimal interaction with H2 blockers because it doesn’t rely heavily on stomach acid or liver enzymes for metabolism. Still, following the 2-hour separation rule is recommended to be safe.
Why was ranitidine pulled from the market?
Ranitidine (Zantac) was removed in 2020 because testing found it contained NDMA, a probable human carcinogen. The levels increased over time, especially when stored at higher temperatures. Even though it was an H2 blocker, its safety risk had nothing to do with drug interactions-it was a contamination issue.


13 Comments
This is the kind of post that saves lives. I work in pharmacy and see people mixing H2 blockers with antivirals all the time. No one tells them the timing matters. Just because it's a 'heartburn pill' doesn't mean it's harmless. I always tell patients: take your antifungal first, wait two hours, then hit the Pepcid. Simple. Life-saving.
Fluconazole and famotidine? Fine together. Itraconazole? Not so much. Keep it simple.
Man I wish I'd known this five years ago. My cousin was on itraconazole for a bad fungal infection and kept getting worse. They kept upping the dose thinking it wasn't working. Turns out she was taking Tagamet every night for her acid reflux. No one ever connected the dots. She ended up in the hospital. I'm telling everyone I know now. This isn't just some obscure drug interaction-it's a silent killer in plain sight. And the fact that 31% of antiviral labels don't even say how to time it? That's wild. Doctors assume patients read the fine print. But most of us just swallow the pills and hope for the best. We need better labeling. Like, mandatory bold warnings with a clock icon or something. People need to see it, not just read it.
In India, many patients self-medicate with over-the-counter famotidine for indigestion without knowing they are on antifungals. This information is critical for community health workers. We must educate not only patients but also local pharmacists who often recommend these combinations unknowingly. The cost of antifungals is already high-adding treatment failure due to poor timing is unacceptable. We need public awareness campaigns in regional languages as well.
My uncle died because of this. Not directly, but indirectly. He had HIV, was on atazanavir, and took Zantac every day because he 'didn't want to feel bloated.' No one told him it was sabotaging his meds. He developed resistance. Then the opportunistic infections came. I still think about it. I swear, if I ever see someone taking H2 blockers with antivirals, I'm gonna pull them aside and scream it into their face. This isn't just science-it's grief waiting to happen.
Let me just say this: if you’re taking cimetidine with anything, you’re either a medical student who hasn’t passed pharmacology yet, or you’re living in 1998. Cimetidine is the grandpa of H2 blockers. It’s got more drug interactions than a bad Tinder date. Famotidine? Clean. Efficient. Modern. And yes, I checked the Liverpool database. 63% vs. 12%. That’s not a coincidence. That’s a red flag with a megaphone. Also, stop calling Zantac ‘safe’-it was a chemical time bomb. NDMA isn’t some ‘maybe’ carcinogen-it’s a proven one. The FDA didn’t pull it because they were bored.
Just had to comment because I’ve been on voriconazole for aspergillosis and was taking Pepcid every night. My doc never mentioned the enzyme thing. I only found out when I googled it after reading this. Got my blood levels checked-was at 6.2 mcg/mL. Way too high. Switched to famotidine and cut the dose to every other night. Now I’m at 4.1. Feels better. No more brain fog. Also, I’m not a doctor but this saved me. Please share this with someone who needs it.
Wow. So H2 blockers are like the quiet roommate who doesn't say much but secretly messes with your wifi password. Famotidine? Quiet but harmless. Cimetidine? Quiet and also deletes your entire hard drive. And PPIs? That’s the roommate who changes the locks and never lets you back in. I love how this post doesn’t just say ‘don’t do it’-it gives you a way out. Timing. That’s the real hero here. Two hours. That’s all it takes. Like waiting for your coffee to cool before you sip it. Simple. Human. Brilliant.
okay so i just realized i’ve been taking my fluconazole with my pepcid at the same time for 3 months because i thought if it’s not ‘strong’ like a ppi then it’s fine. i’m so dumb. but like… why do we even have to memorize this stuff? shouldn’t the pills just have little icons? like a clock and a warning sign? i’m not a pharmacist, i’m just trying to get better. also i love that isavuconazole is the chill new kid who doesn’t care about drama. we need more of those.
Thank you for writing this with such clarity. 💙 As someone who’s been managing chronic fungal infections for years, this is the first time I’ve seen a breakdown that doesn’t feel like reading a textbook. I’ve been using famotidine at night and taking itraconazole in the morning-exactly as you said. It made all the difference. Keep sharing knowledge like this. It matters more than you know.
I work in a clinic and we just started handing out these timing sheets to patients on antifungals. We printed a little card: ‘Antifungal → Wait 2 hours → H2 Blocker.’ Simple. No jargon. Our adherence rate jumped from 38% to 79% in three months. People aren’t dumb-they just need it spelled out. This post? It’s the kind of thing that should be on every pharmacy counter. And maybe even in the waiting room of every infectious disease clinic. We’re all just trying not to die while we’re trying to get better.
Don’t take cimetidine. Ever. With anything. Just… don’t.
bro this is wild 😳 i had no idea famotidine was the ‘good’ h2 blocker. i’ve been taking tagamet for years because it’s cheap. just switched to pepcid today. also isavuconazole sounds like a superhero name 🦸♂️💊. if they make a pill that doesn’t care about stomach acid… i’m buying a lifetime supply. also i’m telling my whole family about this. someone’s life might depend on it 🙏