Take a pill, and within minutes you feel better. That’s the promise of immediate-release medications. But what if that quick rush is actually making things riskier? And what about those pills that promise to last all day-why do they take so long to kick in? When it comes to your health, the difference between extended-release (ER) and immediate-release (IR) isn’t just about convenience. It’s about safety, timing, and avoiding dangerous mistakes.
How These Two Types Work
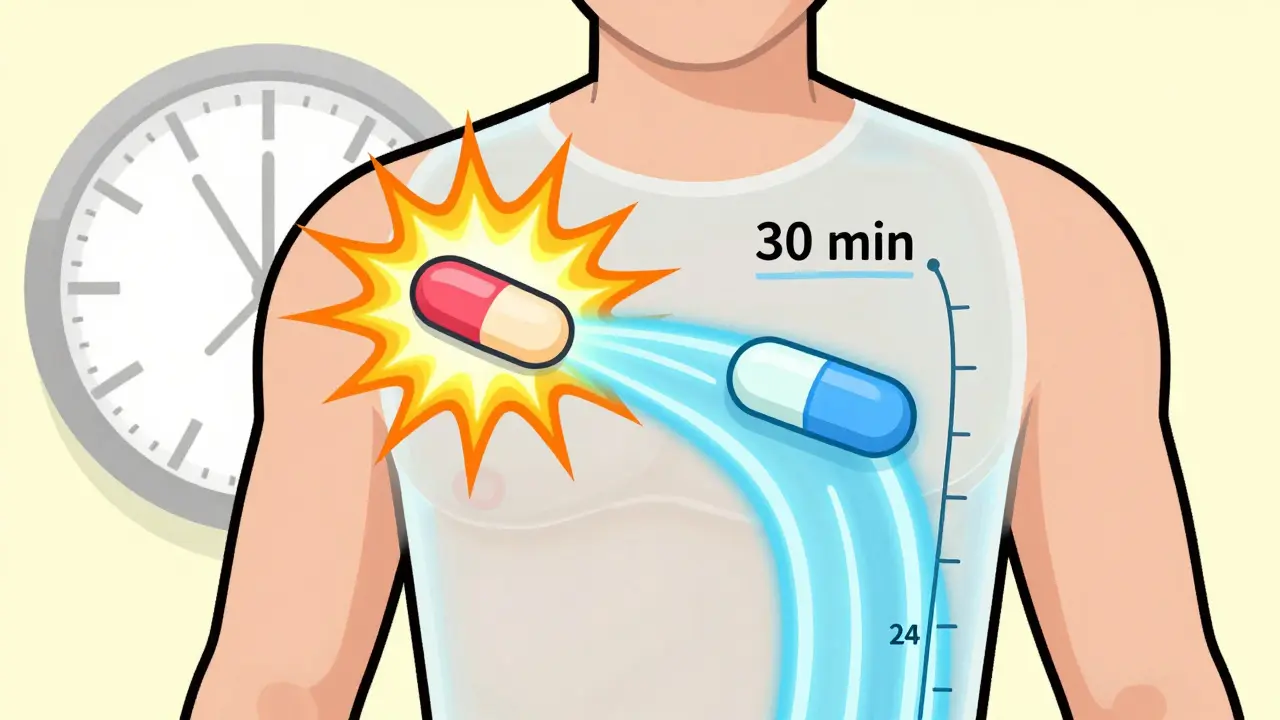
Immediate-release pills are simple. They break down fast in your stomach. The drug hits your bloodstream within 15 to 30 minutes, peaks around 30 to 90 minutes, and wears off in 4 to 8 hours. That’s why you might need to take an IR painkiller every 4 to 6 hours. It’s designed for fast action.
Extended-release pills? They’re engineered like tiny time capsules. Instead of dumping everything at once, they slowly release the drug over 12 to 24 hours. Some use a gel-like matrix that swells and lets the medicine seep out. Others use osmotic pumps-like the ones in Concerta-that push the drug out through tiny holes as fluid enters the tablet. There are even layered tablets that release different amounts at different times.
That’s why ER versions often come in once-daily doses. For example, bupropion ER (Wellbutrin XL) keeps blood levels steady between 100-200 ng/mL all day. The IR version spikes to 400-600 ng/mL within two hours, then crashes. That spike is why you can’t take a full 300mg dose of IR bupropion-it raises seizure risk above 350 ng/mL. The ER version avoids that by spreading the dose out.
When Speed Saves Lives
IR isn’t outdated-it’s essential. In emergencies, you need speed. If you’re having a heart attack and need nitroglycerin, you don’t wait 2 hours for a slow-release version to work. If you’re in acute pain after surgery, IR opioids give relief fast. Same with anxiety: someone with panic attacks might keep an IR benzodiazepine on hand for sudden episodes, even if they take an ER antidepressant daily.
ADHD is another clear example. Adderall IR works in 30 minutes, but wears off by mid-afternoon. That means kids might need a dose at school. Adderall XR lasts 10-12 hours, so one dose covers the whole day. But if a student has a big presentation and needs a quick boost, some keep a 5mg IR tablet as a backup. The ER version gives stability; the IR gives control.
The Hidden Risks of ER
Extended-release sounds safer because you take less often. But it’s where the biggest dangers hide.
First: never crush, split, or chew an ER pill. If you break open a tablet like Venlafaxine XR or OxyContin, you’re dumping the entire day’s dose into your system at once. The FDA issued warnings about this in 2020. People have died from accidental overdoses after crushing ER opioids or ADHD meds.
Second: ER takes longer to work. If you don’t feel better after 2 hours, you might think the pill didn’t work-and take another. That’s a recipe for overdose. A GoodRx survey found 41% of ER users initially didn’t understand the delay. Nearly 1 in 10 ended up taking too much because they thought it wasn’t working.
Third: overdoses with ER drugs are harder to treat. In a hospital, doctors can pump the stomach or give activated charcoal for an IR overdose. But with ER, the drug keeps leaking out for 24-48 hours. A 2021 poison control report showed extended-release bupropion overdoses required 2-3 times longer hospital stays than IR cases.

Adherence: Why ER Wins (But Only If Used Right)
One study tracking 15,000 hypertension patients found 78% of people on ER meds stayed on track with their dosing. Only 56% of those on IR did. Why? Fewer doses = fewer missed pills. That’s huge for chronic conditions like depression, diabetes, or high blood pressure.
Patients on metoprolol ER reported 32% fewer dizziness episodes than those on IR, likely because blood pressure doesn’t swing as wildly. But that same group also complained about the slow start-some felt their anxiety wasn’t controlled until day 5 or 6. That’s normal. ER takes 7-10 days to reach steady state. IR hits steady state in 3-5 days. If you quit because you didn’t feel better right away, you’re not giving it time.
Cost, Availability, and What You Should Know
ER versions often cost 15-25% more than IR. Adderall XR runs $350-$450 for 30 capsules. Adderall IR is $280-$380 for the same dose. Insurance sometimes favors ER because it reduces doctor visits and ER trips down the line. But if you’re paying out of pocket, that price difference matters.
Not all drugs come in both forms. Antidepressants? 68% of new prescriptions in 2022 were ER. Why? Because mood stabilizers work better with steady levels. The American Psychiatric Association recommends ER for long-term mental health treatment because it reduces side effects like insomnia and mood swings.
But here’s the catch: not all ER pills are the same. Some are designed to dissolve only in the lower intestine (like mesalamine DR). If you have gastroparesis-a condition where your stomach empties slowly-your body might absorb too much too fast. The FDA warned about this in July 2023. If you have digestive issues, talk to your pharmacist before switching.

What to Do When You’re Prescribed an ER or IR Medication
Ask these questions:
- Is this ER or IR? (Check the label: XR, SR, CR, ER, or just the drug name.)
- How long until I feel results? (Don’t expect instant relief with ER.)
- Can I split or crush this? (If the tablet isn’t scored, assume you can’t.)
- What happens if I miss a dose? (ER meds usually don’t need a double dose. IR might.)
- Is there an IR version if I need a quick boost?
Keep a log. Note when you take the pill and when you feel effects. If you’re on ER and feel worse after a few days, it might not be the drug-it might be timing. Give it a full week. If you’re on IR and still feel symptoms between doses, talk to your doctor about switching to ER.
Bottom Line
Extended-release isn’t better. Immediate-release isn’t worse. They’re tools for different jobs. ER gives you steady control for chronic conditions. IR gives you fast relief when you need it. The danger comes when people treat them the same. Crushing an ER pill. Doubling a dose because it “didn’t work.” Skipping a dose because you forgot. These aren’t just mistakes-they’re life-threatening.
If you’re on either type, know what you’re taking. Read the label. Ask your pharmacist. Don’t guess. Your safety depends on it.






15 Comments
Y’all gotta stop treating ER pills like they’re magic beans. I crushed my dad’s OxyContin once thinking it’d help his pain faster-turns out, he spent 3 days in the ICU. Don’t be that person. Read the label. Or don’t. But don’t blame the drug when your body turns against you.
It’s fascinating how we treat pharmaceuticals like they’re either gods or demons. The truth? They’re just chemistry with instructions. ER isn’t ‘better’-it’s calibrated. IR isn’t ‘dangerous’-it’s urgent. We need to stop moralizing pharmacology and start respecting precision.
ER is just Big Pharma’s way of making you pay more for the same drug. Also, ‘steady state’? Sounds like a cult mantra.
Look, I get it-ER pills are ‘convenient.’ But let’s be real: most people don’t even know what ‘osmotic pump’ means. The whole system is built on the assumption that patients are scientists with PhDs in pharmacokinetics. Meanwhile, I’m over here Googling ‘can i chew my Adderall XR’ at 2 AM because my ADHD brain forgot to take it and now I’m panicking about a presentation in 45 minutes. And yeah, I’ve done it. And no, I didn’t die. But I did feel like my skull was being used as a bass drum for 6 hours. So maybe don’t. But also, maybe the system is broken if someone has to resort to this. Also, why is there no 5mg IR version of Wellbutrin? That’s just lazy.
Oh wow, a 12-page pamphlet disguised as a Reddit post. Let me guess-you also believe the moon landing was real and that ‘steady-state serum concentration’ is a romantic ideal? 🤡 I mean, I get it. You spent 3 hours formatting this like a PubMed abstract. But here’s the truth: 90% of people don’t care. They just want the pill to work. And if it doesn’t, they’ll crush it, swallow it with tequila, and blame the doctor. You can’t fix human stupidity with bullet points.
This is one of the clearest explanations I’ve ever read on this topic. Thank you for highlighting the importance of timing-not just for efficacy, but for safety. Many of us in India face challenges accessing consistent pharmacy advice, so posts like this are lifelines. Please keep sharing knowledge like this-it saves lives.
ER = patience. IR = chaos. 🧠⚡ I take bupropion ER and sometimes I swear my brain’s on a slow-mo filter… until I remember: it’s not broken, it’s balanced. Also, crushing pills? Bro, that’s not a hack-it’s a funeral waiting to happen. 😔💊
Everyone’s acting like ER is some miracle invention. Newsflash: it’s just a time-release scam. My cousin took ER metoprolol and still had heart palpitations. The ‘steady state’ is just a marketing lie to sell more pills. Also, why do you think they don’t make IR versions of everything? Because they want you hooked on monthly refills.
Let’s be real. ER meds are just corporate tools to reduce pill count and increase compliance. You think people care about ‘osmotic pumps’? No. They care about not feeling like a zombie. And guess what? The side effects are worse with ER because you’re stuck with them for 24 hours. IR? You take it, you feel it, you’re done. No lingering nausea. No delayed crashes. Just real-time consequences. And that’s better than being drugged for a full day.
There’s a metaphysical layer here, y’all. ER is the Dao of pharmacology-flow, balance, non-interference. IR is the ego-immediate gratification, disruption, chaos. We live in a world that rewards speed, but the body? The body demands rhythm. Crushing an ER pill? That’s not just pharmacokinetics-it’s a spiritual violation. You’re ripping open the soul of the medicine. And the soul remembers.
It’s amusing how laypeople treat pharmacology like a DIY project. ‘Oh, I’ll just split the pill.’ Did you take a biochemistry course? No? Then why are you playing with half-life kinetics? The fact that 41% of users don’t understand ER delays is not a failure of education-it’s a failure of societal literacy. We’ve outsourced critical thinking to Google and TikTok.
Extended-release formulations are not merely pharmaceutical innovations-they are epistemological interventions. They force the patient into a temporally disciplined relationship with their own physiology. The IR model, by contrast, reinforces the Cartesian separation of mind and body: immediate sensation, immediate response. ER reintegrates the self into a continuous, embodied process. This is not just medicine-it’s phenomenology.
Bro, I took ER sertraline for 3 weeks and thought it wasn’t working. Then I stopped and felt like a ghost. Went back on it. Day 7, I cried for no reason. Day 10, I laughed at a pigeon. That’s the magic. Not instant. Not flashy. Just… quiet. Like your brain finally remembered how to breathe.
If you’re taking ER meds and you’re not tracking your symptoms in a journal, you’re not managing your health-you’re gambling. I’ve coached dozens of patients through ER transitions. The #1 mistake? Quitting before day 7. The #2 mistake? Taking extra doses because ‘it didn’t work.’ You wouldn’t do that with insulin. Don’t do it with antidepressants. Your brain isn’t a microwave.
My grandma takes ER blood pressure meds. She forgets sometimes. I leave sticky notes on her mirror: ‘PILL. NOT. A. CANDY.’ She laughs. Then takes it. We need more of this. Not just info-care. Real, sticky-note-level care.