Renal Dose Calculator for Chronic Kidney Disease
Input Patient Data
Results
Dosing Recommendations
- For medications with >50% renal clearance, consider dose reduction
- Monitor for toxicity with drugs like vancomycin, aminoglycosides, and metformin
- Avoid NSAIDs in stages 3-5 CKD
- When eGFR < 30 mL/min, consider dosing intervals every 48-72 hours for vancomycin
Critical Warnings:
Avoid ACE inhibitors/ARBs with NSAIDs - risk of AKI increases five-fold
Never assume "low-risk" drugs are safe for renal patients
Remember to adjust for weight changes in dosing calculations
When a patient has chronic kidney disease a progressive loss of kidney function that reduces the body's ability to filter and eliminate drugs, medication handling changes dramatically. The kidneys normally clear about 30% of all medicines, so any drop in filtration can turn a routine prescription into a toxic surprise.
Key Takeaways
- Even modest CKD (eGFR < 60 mL/min/1.73 m²) forces dose cuts for roughly 40% of common drugs.
- NSAIDs, calcineurin inhibitors, metformin, certain DOACs, sulfonylureas, trimethoprim and vancomycin are the biggest culprits.
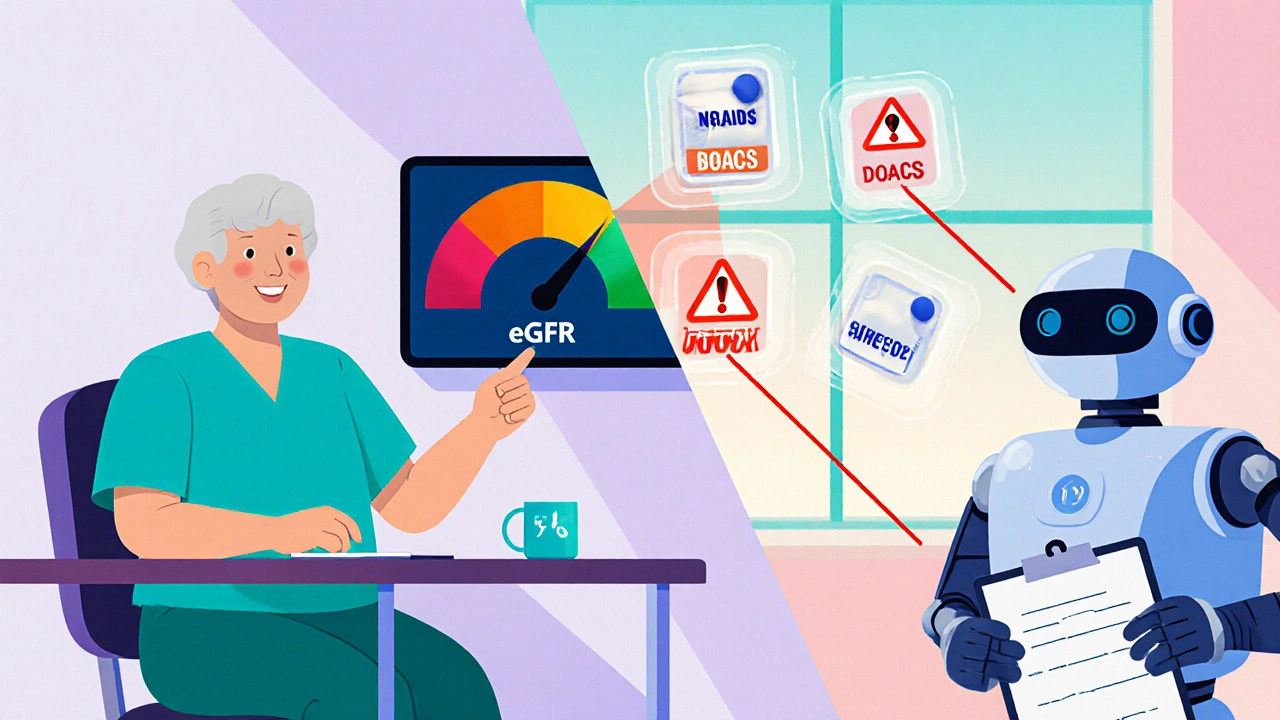
- Use eGFR, not just serum creatinine, to decide when to adjust or stop a drug.
- Tools like the Cockcroft‑Gault formula, KDIGO guidelines, and the KidneyIntelX platform cut adverse events by up to 63%.
- Preventable drug‑induced AKI adds $10‑15 k per hospital stay; proper dosing saves lives and money.
Why Kidney Disease Alters Drug Clearance
The kidneys eliminate drugs through three main routes:
- Glomerular filtration - filtered directly into urine.
- Tubular secretion - active transport pumps move drug molecules from blood into the tubule.
- Metabolism within renal cells - some drugs are broken down before excretion.
When eGFR estimated glomerular filtration rate, the clinical gauge of kidney function falls below 60 mL/min/1.73 m² (CKD stage 3), each of these pathways slows down. The result is higher plasma concentrations, longer half‑lives, and, in the worst case, toxicity.
High‑Risk Medication Classes
Not all drugs behave the same in CKD. Below is a quick guide to the families most likely to accumulate.
| Drug class | Typical renal clearance | Key toxicity in CKD | eGFR trigger for adjustment |
|---|---|---|---|
| NSAIDs (ibuprofen, naproxen, diclofenac) | Minimal - effect via prostaglandin inhibition | Acute kidney injury, fluid overload | <60 mL/min |
| Calcineurin inhibitors (tacrolimus, cyclosporine) | ~30% | Vasoconstriction, interstitial fibrosis | <30 mL/min |
| Metformin | ~30% (unchanged) | Lactic acidosis | <45 mL/min (dose reduction); <30 mL/min (stop) |
| DOACs (apixaban 50%, rivaroxaban 33%) | Renal‑dependent | Bleeding | <30 mL/min (dose cut) ; <15 mL/min (avoid) |
| Sulfonylureas | Varies - chlorpropamide 100%, glyburide 20% renal | Severe hypoglycemia | <30 mL/min (avoid chlorpropamide/glyburide) |
| Trimethoprim (co‑trimoxazole) | ~30% | Hyperkalemia, especially with ACE‑I/ARB | <60 mL/min |
| Vancomycin | ~70% | Nephrotoxicity, ototoxicity | <30 mL/min (extend interval) |
| Aciclovir | ~90% | Crystal nephropathy, seizures | <50 mL/min (dose cut) |
How to Adjust Doses Safely
The most reliable way to decide on a dose change is to calculate creatinine clearance. Two formulas dominate:
- Cockcroft‑Gault - uses age, weight, gender, and serum creatinine; favored for drug‑level monitoring.
- CKD‑EPI equation - provides an eGFR that matches KDIGO staging; best for overall kidney assessment.
Once you have the number, follow the KDIGO guidelines the international standard for kidney disease management released in 2023. They recommend reviewing every medication when eGFR drops below 60 mL/min and making dose cuts or substitutions for drugs with >50% renal clearance.
Example - Vancomycin: The standard 15 mg/kg every 12 hours becomes 15 mg/kg every 48‑72 hours when eGFR is under 30 mL/min, and you must aim for trough levels of 15‑20 µg/mL instead of the usual 10‑15 µg/mL.
Common Pitfalls and How to Avoid Them
Even experienced clinicians slip up. The biggest errors are:
- Relying on a single serum creatinine value without converting to eGFR - about 35% of primary‑care visits miss this step.
- Assuming a drug is safe because it’s “low‑risk” without checking renal clearance - 42% of dose‑related errors involve >50% renal‑cleared drugs.
- Prescribing NSAIDs together with ACE‑I or ARB - this combo spikes AKI risk five‑fold.
- Forgeting to adjust for weight changes in the Cockcroft‑Gault calculation - a 10 kg loss can overestimate clearance by 15%.
Solutions include automated eGFR alerts in electronic health records, using decision‑support apps like Meds & CKD, and involving pharmacists in the medication‑review process.
Economic and Clinical Impact
Drug‑induced AKI adds $10‑15 k per admission, and 38% of those cases are preventable with proper dosing. Medicare data shows CKD patients on ten or more meds have 2.3 × the hospitalization rate of those on fewer drugs, accounting for an extra $18.7 billion in annual costs.
Regulators are responding. The FDA now requires renal dosing information on every new drug label, issuing $2.5 million fines for non‑compliance. In Europe, the EMA recorded over 12 k cases of drug‑related kidney injury in 2022, nearly half linked to dosing errors.

Future Directions: AI and Precision Medicine
The newest tool on the block is KidneyIntelX an AI platform that predicts individualized medication toxicity in CKD patients. In a 10 000‑patient validation study, it correctly flagged high‑risk prescriptions 89% of the time, cutting adverse events by 63% when clinicians acted on its alerts.
Ongoing trials are testing pharmacogenomic‑guided dosing, which could further reduce toxicity by matching drug choice to a patient’s genetic makeup. Within five years, experts predict that EHRs will auto‑flag any renally cleared medication that exceeds the safe dose for a given eGFR, trimming dosing errors by three‑quarters.
Practical Checklist for Clinicians
- Calculate eGFR (CKD‑EPI) at every visit for patients with known CKD.
- Review the medication list for >50% renal clearance drugs.
- Apply KDIGO dose‑adjustment tables - if unsure, halve the dose and monitor levels.
- Avoid NSAIDs and consider alternative pain relievers (e.g., acetaminophen) in stages 3‑5.
- Stop metformin when eGFR < 30 mL/min; reduce dose if 30‑45 mL/min.
- When prescribing DOACs, select agents with lower renal clearance (e.g., apixaban) and adjust dose per eGFR.
- Use pharmacist‑led medication reconciliation for patients on ≥10 drugs.
- Leverage decision‑support tools (Meds & CKD, KidneyIntelX) for real‑time alerts.
Frequently Asked Questions
How often should eGFR be checked in CKD patients?
At least twice a year for stage 3, every 3‑6 months for stages 4‑5, and before starting or changing any renally cleared medication.
Can over‑the‑counter pain relievers be safe?
Acetaminophen is generally safe up to 2 g per day in CKD. NSAIDs should be avoided once eGFR falls below 60 mL/min because they sharply raise AKI risk.
Is metformin completely banned in CKD?
No. Reduce the dose when eGFR is 30‑45 mL/min and stop it entirely below 30 mL/min to prevent lactic acidosis.
What is the safest anticoagulant for a patient with eGFR 20 mL/min?
Apixaban, which is 50% renally cleared, can be used at a reduced dose (2.5 mg bid) if the patient meets dose‑reduction criteria. Warfarin remains an alternative because it is non‑renal.
How does hyperkalemia develop with trimethoprim?
Trimethoprim blocks renal tubular potassium secretion. When combined with ACE‑I or ARB, potassium can rise 1.2‑1.8 mmol/L within 48 hours, leading to dangerous arrhythmias.
Understanding the link between kidney disease and drug accumulation is essential for keeping patients safe. By using eGFR‑based dosing, following KDIGO recommendations, and leveraging modern decision‑support tools, clinicians can dramatically cut toxicity rates and improve outcomes.






13 Comments
Thanks for putting together such a thorough overview.
Renal clearance hinges on glomerular filtration coefficiency and tubular secretory transporters. When eGFR drops below 60ml/min the substrate concentration gradient shifts causing accumulation of high‑clearance drugs. NSAIDs for example inhibit prostaglandin synthesis which further compromises renal perfusion. Calcineurin inhibitors like tacrolimus are metabolized partially renally and require therapeutic drug monitoring. Metformin’s lactate pathway becomes impaired and the risk of lactic acidosis spikes dramatically. Direct oral anticoagulants such as apixaban have renal‑dependent half‑lives that must be adjusted per KDIGO tables. Sulfonylureas with high renal clearance can precipitate severe hypoglycemia if dose is not reduced. Trimethoprim competitively blocks epithelial sodium channels leading to hyperkalemia especially with ACE‑I co‑therapy. Vancomycin dosing intervals should be extended once clearance falls under 30ml/min to avoid nephrotoxicity. The Cockcroft‑Gault formula remains the gold standard for creatinine‑clearance estimation in drug dosing. Decision‑support platforms embed these algorithms and flash alerts when a prescription exceeds the renal limit. Studies show AI‑driven alerts cut adverse drug events by up to 63% in CKD cohorts. Clinicians should verify eGFR at each visit and cross‑check against medication lists before any new order. Automating the reconciliation process reduces human error and saves thousands of dollars per admission. Bottom line keep the dosing conservative and monitor serum levels whenever possible 😊
If you’re juggling ten or more meds in a CKD patient, you’re basically walking a tightrope. The checklist you posted is spot‑on, especially the reminder to halve doses when you’re unsure. I’ve seen cases where a simple switch from ibuprofen to acetaminophen prevented a whole cascade of AKI episodes. Remember that weight fluctuations can throw off Cockcroft‑Gault estimates, so re‑measure weight regularly. Pharmacist‑led medication reviews have been shown to slash hospital readmissions by nearly a third in real‑world studies. Keep pushing these best practices and you’ll save lives and some serious healthcare dollars.
Checking eGFR every three months for stage 4 patients is a no‑brainer. Adjust the dose once the number dips below the threshold you listed. Using the KDIGO table is straightforward and saves time. Avoid NSAIDs altogether when eGFR is under 60. Simple steps make a big difference.
Listen, if you’re still prescribing metformin at an eGFR of 25 ml/min you’re courting disaster. Drop the drug immediately and switch to a dose‑adjusted alternative. For anticoagulation choose apixaban at the reduced dose or go back to warfarin with INR monitoring. Never combine an NSAID with an ACE‑I in CKD – it’s a recipe for AKI. Use the KidneyIntelX alerts; they’ll flag risky combos before you hit the pharmacy. Stay vigilant, the numbers don’t lie.
That can be overwhelming when you’re trying to keep up with appointments. I’ve found that setting a reminder in the EMR to run eGFR checks helps keep the process smooth. Talking to patients about why a dose is being cut also builds trust. It’s okay to lean on pharmacists for a second opinion. Small changes add up to better outcomes.
All this hype about AI alerts is overblown; clinicians have been managing dosing long before any algorithm existed. Relying on a black‑box system erodes professional judgment and creates complacency. The real issue is that doctors aren’t trained enough in pharmacokinetics. If you keep outsourcing to software you’ll never learn the fundamentals. Stick to the basics and don’t let a dashboard dictate care.
Your argument presupposes that electronic decision‑support is infallible, yet numerous studies have documented false‑positive alerts resulting in unnecessary dose reductions. Moreover, the pharmacodynamic variability among patients with chronic kidney disease necessitates individualized assessment beyond algorithmic thresholds. It is therefore prudent to employ such tools as adjuncts rather than replacements for clinical expertise. Comprehensive evaluation should incorporate laboratory trends, comorbid conditions, and patient‑specific factors before modifying therapy.
Okay, let’s break this down. The data on drug‑induced AKI is solid – you can’t argue with the numbers. But the way the guidelines are written sometimes feels like a maze. If you just follow the eGFR cutoffs you’ll miss nuances like the impact of concurrent diuretics. I’d say keep a spreadsheet of your high‑risk meds and cross‑reference each new prescription. It’s not glamorous, but it works.
One must consider the broader context wherein pharmaceutical companies exert undue influence over dosing recommendations, subtly steering clinicians toward more profitable regimens. The FDA’s recent mandate for renal information on labels, while ostensibly beneficial, could also serve as a veneer for delayed scrutiny of off‑label uses. It is incumbent upon us to remain vigilant and interrogate the data sources that inform our practice. 🕵️♀️ The integration of AI platforms, such as KidneyIntelX, may mask algorithmic biases that favor certain drug manufacturers. Therefore, a critical appraisal of each alert is essential before implementation.
Picture this: a patient walks into the ER with a serum potassium of 6.8 mmol/L, the result of an unchecked trimethoprim prescription. The cascade that follows-cardiac arrhythmia, ICU admission, skyrocketing bills-is a direct consequence of neglecting renal dosing. Every missed eGFR check is a ticking time bomb. The statistics aren’t just numbers; they’re lives hanging in the balance. When the decision‑support system finally beeps, it’s often too late to prevent the fallout. That’s why preemptive dose adjustment isn’t optional-it’s a moral imperative.
I agree with the points raised about pharmacist involvement. Their expertise adds a safety net that many clinicians lack time for. Implementing routine medication reconciliation can be done without overhauling the workflow. Small collaborative steps lead to big improvements.
Honestly, if doctors dont take the time to calculate crcl correctly theyre just playing with patient lives. It's not just a minor oversight its a breach of trust. We need stricter oversight and maybe some penalties for repeated dosing errors. The system should hold them accountable.