Using an insulin pump isn’t like switching from a flip phone to a smartphone. It’s more like learning to fly a plane - one small mistake can have serious consequences. Continuous Subcutaneous Insulin Infusion (CSII), or insulin pump therapy, gives you precise control over your insulin delivery, but only if you understand how to set it up and keep it safe. If you’re considering a pump or just started using one, getting the settings right isn’t optional. It’s the difference between stable blood sugars and a trip to the ER.
How Insulin Pumps Work - No Fluff, Just the Essentials
Insulin pumps deliver rapid-acting insulin - like Humalog or Novolog - through a tiny tube under your skin. There’s no long-acting insulin involved. Instead, the pump mimics your pancreas by giving you two types of insulin: a steady background dose (basal) and extra doses (bolus) for meals or high blood sugar.
The pump runs 24/7. If it stops working - say, the tubing kinks or the battery dies - your body stops getting insulin. That’s not a glitch. That’s a medical emergency. Diabetic ketoacidosis (DKA) can develop in as little as 2 to 4 hours if insulin delivery is interrupted. This isn’t theory. It’s what happens in real life, and it’s why every pump user needs to know how to spot and fix a problem fast.
Basal Rates: The Foundation of Safe Pump Therapy
Your basal rate is the invisible backbone of your insulin plan. It’s the tiny amount of insulin your pump delivers every hour to keep your blood sugar steady between meals and while you sleep. Most people need different basal rates at different times. For example, you might need more insulin at 3 a.m. because of the dawn phenomenon, and less after a workout.
Typically, basal insulin makes up 40% to 50% of your total daily dose. But that’s just a starting point. The real test is a fasting basal test. You skip breakfast, lunch, and dinner. You don’t exercise. You check your blood sugar every 2 hours. If your numbers stay within 1 mmol/L (18 mg/dL) of your target, your basal is set right. If it climbs, you need more. If it drops, you need less.
Most modern pumps let you program up to 24 different basal rates. Some even let you save profiles - one for weekdays, one for weekends, one for illness. Use them. Don’t just use the same rate all the time.
Insulin-to-Carbohydrate Ratio and Correction Factor
Now for the mealtime stuff. The insulin-to-carbohydrate ratio (ICR) tells you how many grams of carbs one unit of insulin covers. A common starting point is 1:10 - meaning one unit covers 10 grams of carbs. But that’s not universal. Some people need 1:15. Others need 1:6, especially if they’re very insulin sensitive.
Your correction factor (also called insulin sensitivity factor) tells you how much one unit of insulin lowers your blood sugar. A typical value is 1:3 mmol/L (1:50 mg/dL). So if your blood sugar is 12 mmol/L and your target is 6 mmol/L, you’re 6 mmol/L high. Divide that by 3 - you need 2 units to bring it down.
These numbers aren’t magic. They’re personal. If you’re consistently high after meals, your ICR might be too high (you’re not giving enough insulin). If you’re crashing 3 hours after eating, your ICR might be too low (you’re giving too much). Track your meals and blood sugars for 3 days. Look for patterns. Adjust one thing at a time.
Bolus Types: When to Use Immediate, Extended, or Dual-Wave
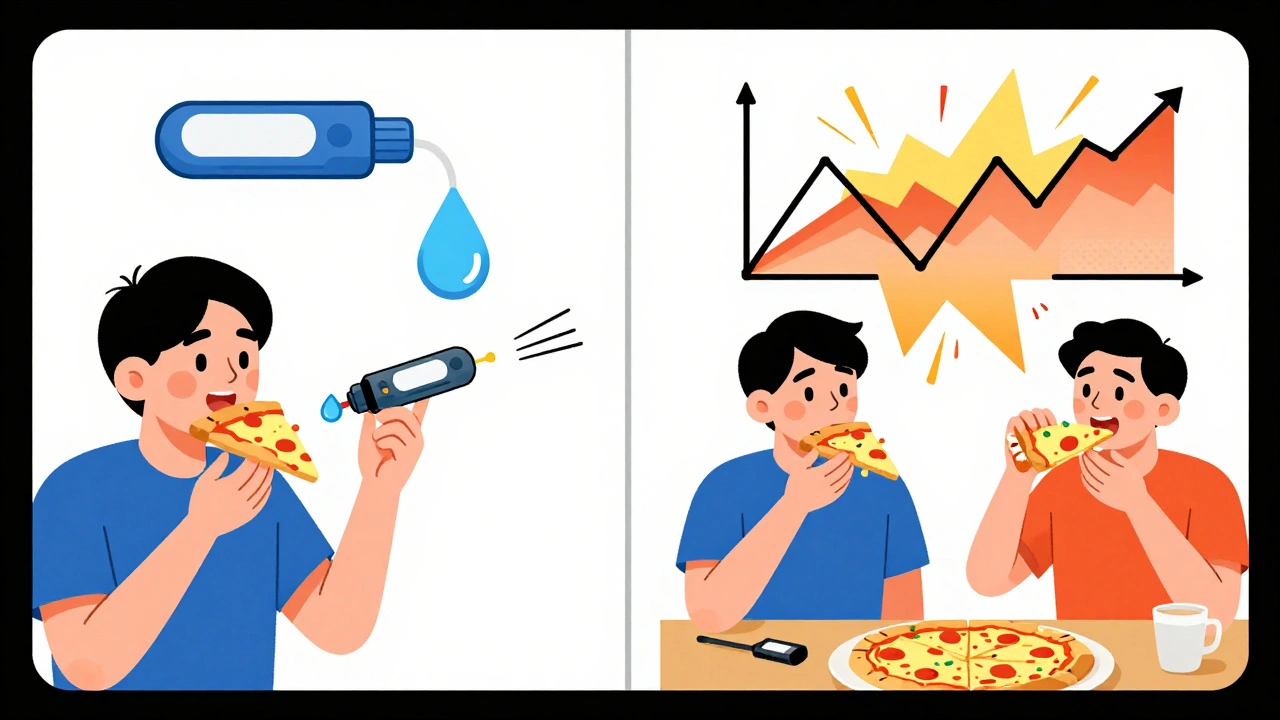
Not all meals are created equal. A bowl of rice? That’s fast-digesting carbs. A pizza? That’s fat and protein slowing down digestion. If you give all your insulin upfront for pizza, you’ll crash later and spike now.
That’s where extended and dual-wave boluses come in.
- Immediate bolus: Use for meals high in carbs and low in fat/protein - like toast, fruit, or pasta.
- Extended bolus: Use for high-fat meals like pizza, burgers, or creamy pasta. Deliver 50-70% of the insulin upfront, and the rest over 2-4 hours.
- Dual-wave bolus: Combine both. Give 60% right away, and the other 40% over 3 hours. Works well for meals with mixed carbs, fat, and protein.
Many pump users don’t use these features. That’s why they’re constantly adjusting insulin doses manually. Once you start using extended boluses for fatty meals, your post-meal spikes drop - fast.
Infusion Sets and Site Care: Don’t Ignore the Basics
Your pump’s weakest link isn’t the software. It’s the tubing and the site where it enters your body. Change your infusion set every 2 to 3 days. No exceptions. Leaving it in longer increases your risk of infection, poor insulin absorption, and lipohypertrophy - lumpy scar tissue that blocks insulin from working.
Rotate your sites: abdomen, thighs, upper arms, lower back. Avoid the same spot two days in a row. If you notice redness, swelling, or pain, change the site immediately. Don’t wait. A minor irritation today can become a serious infection tomorrow.
And always have a backup. Keep extra infusion sets, insulin, batteries, and glucagon on hand. You never know when the pump will fail.
Safety First: What Happens When Things Go Wrong
Here’s the hard truth: pumps can fail. Tubing can kink. The battery can die. The cannula can pop out. And if you don’t notice, your body goes without insulin - fast.
Signs of pump failure:
- Blood sugar rising over 13 mmol/L (234 mg/dL) with no clear reason
- High ketones in your blood or urine
- Unexplained nausea, vomiting, or abdominal pain
- Pump alarm going off and you don’t know why
If you suspect a problem, do this:
- Check your tubing for kinks or air bubbles.
- Check your insulin reservoir - is it empty?
- Check your battery.
- If all looks good but your sugar is still rising, disconnect the pump.
- Give yourself a correction dose of insulin with a syringe or pen.
- Call your diabetes team.
Never assume the pump is working just because it’s beeping. Beeping doesn’t mean delivering. Always verify with your blood sugar.
Pump Use During Illness, Surgery, and Pregnancy
Illness changes your insulin needs. Stress hormones spike your blood sugar. You might need 20-50% more insulin than usual. Keep checking every 2-4 hours. Don’t skip boluses just because you’re not eating. Your body still needs insulin.
For minor surgery - like a dental procedure - your pump can stay on if your blood sugar is between 4 and 12 mmol/L, your reservoir is full, and the site is accessible. For major surgery or anything requiring fasting longer than 3 hours, switch to IV insulin. Your care team will handle this. Don’t guess.
After giving birth, your insulin needs drop sharply. Many women need 30-50% less insulin right after delivery. If you’re breastfeeding, you’ll need even less - another 10-20% reduction. Your pump settings must change. Don’t wait for your next appointment. Adjust now.

Advanced Features: Closed-Loop and Interoperability
Some pumps today are hybrid closed-loop systems - like the Medtronic 670G or Tandem Mobi. They automatically adjust your basal insulin based on your CGM readings. But they still need you to tell them when you eat. They’re not magic. They’re tools.
The big shift? Interoperability. Older pumps only worked with one brand’s CGM. Now, pumps like the Omnipod 5 can talk to Dexcom, Freestyle Libre, and others. That means more choice. More flexibility. More control.
But don’t let tech distract you from the basics. A fancy pump won’t fix bad carb counting. It won’t fix skipped site changes. It won’t fix ignoring high ketones.
Who Shouldn’t Use a Pump - And Why
Not everyone should use a pump. The American Diabetes Association says you need to be able to:
- Check your blood sugar at least 4 times a day
- Count carbs accurately
- Understand how insulin works
- Respond to high and low blood sugars
- Handle technical issues without panicking
If you can’t do these things, a pump isn’t safer. It’s riskier. People with severe hypoglycemia unawareness should only use pumps with automatic low-glucose suspend - and even then, only with a CGM.
And if you’re unwilling to learn? Don’t start. It’s not worth the danger.
Real User Experiences - What Works and What Doesn’t
People who succeed with pumps do three things:
- They track everything - meals, carbs, blood sugar, insulin.
- They change their infusion sets religiously - every 48 hours, no exceptions.
- They test their basal rates regularly - at least once every 3 months.
Those who struggle? They skip site changes. They guess their carb counts. They ignore alarms. One user on Reddit said: "I went into DKA because I thought the pump was just being annoying. Turns out, the tubing was blocked for 6 hours. I almost died."
Another said: "I dropped my A1c from 8.9% to 6.8% in 5 months - not because of the pump, but because I finally started counting carbs properly. The pump just made it easier to see the results."
The pump doesn’t fix your habits. It exposes them.
Final Advice: Master the Basics Before You Chase the Fancy
There’s no shortcut. No magic setting. No app that replaces your brain.
If you want to succeed with insulin pump therapy:
- Learn your basal rates inside out.
- Use extended boluses for fatty meals.
- Change your site every 2-3 days.
- Carry backup insulin and glucagon.
- Test your settings every few months.
- Don’t ignore high blood sugar - even if the pump says it’s "fine."
Insulin pumps are powerful. But they’re not smarter than you. They’re just faster. And if you’re not paying attention? They’ll deliver insulin - even when you shouldn’t have any.
Can I swim or shower with my insulin pump?
Most pumps are water-resistant but not waterproof. You can shower with most modern pumps, but swimming usually requires disconnecting. Always check your pump’s manual. If you disconnect, give yourself a bolus to cover the time you’re off, especially if you’re active. Never leave the pump disconnected for more than 1 hour without replacing the insulin with a shot.
How often should I check my pump settings?
Check your basal rates and insulin-to-carb ratios every 3 months, or sooner if your weight, activity level, or health changes. If you’re sick, pregnant, or starting a new medication, test them immediately. Use your pump’s download feature to review your glucose trends and insulin delivery patterns. If you’re consistently high or low at certain times, your settings need adjusting.
What should I do if my pump stops working during the night?
If you wake up with high blood sugar and suspect pump failure, don’t wait. Check your tubing, reservoir, and battery. If everything looks fine but your sugar is rising, disconnect the pump and give yourself a correction dose with a syringe or pen. Use your insulin sensitivity factor to calculate the dose. Call your diabetes team in the morning. Never try to "wait it out." High blood sugar overnight can lead to DKA.
Is it safe to use an insulin pump during pregnancy?
Yes - and many women find pumps help them achieve tighter blood sugar control during pregnancy, which reduces risks to the baby. But your insulin needs will change drastically. In the first trimester, you may need less insulin. In the second and third, you’ll need much more. Work closely with your endocrinologist and diabetes educator. Adjust basal rates and bolus ratios weekly. Use a CGM to catch highs and lows early.
Why do I keep getting high blood sugar after changing my infusion site?
It’s common. When you change your site, your body needs time to absorb insulin properly. Give it 2-4 hours before expecting full effect. If you’re still high after 4 hours, you may have inserted into scar tissue or fat that doesn’t absorb well. Try a different site. Always rotate locations. If you’re consistently high after site changes, your basal rate might be too low. Test it with a fasting basal test.






15 Comments
I switched to a pump last year and honestly? The biggest game-changer was learning to use extended boluses for pizza. I used to crash at 2 a.m. Now I sleep through the night. No more 3 a.m. glucose checks.
Also, changing my site every 48 hours like clockwork? Non-negotiable. I used to stretch it to 5 days and wonder why my sugars were all over the place. Duh.
I find it deeply concerning that this article casually dismisses the systemic failures of medical infrastructure that render insulin pumps inaccessible to vast populations. The privilege embedded in assuming everyone has access to CGMs, backup insulin, and diabetes educators is not merely negligent-it is ethically indefensible.
Okay but let’s be real-this isn’t about pumps. It’s about metabolic autonomy. The fact that we’re still treating insulin delivery like a DIY plumbing project instead of a neurofeedback-integrated bio-system is wild. I mean, have you seen the latest Dexcom G7 integration with the Omnipod 5? It’s not just tech. It’s transcendence.
Also, if you’re not using dual-wave for tacos, you’re doing it wrong. Just saying.
Yeah, I tried the pump. Lasted three weeks. Turned out I just needed to eat less bread.
The emphasis on basal rate testing is absolutely critical. I conducted a 24-hour fasting test last month and discovered my overnight basal was 0.4 units/hour too high-resulting in recurrent hypoglycemia between 2 and 4 a.m. After adjusting, my fasting A1c dropped 0.7% in six weeks. Precision matters. Every decimal point counts.
Also, rotating infusion sites is not optional. Lipohypertrophy is a silent killer. Document your sites. Use a grid. Track it like a scientist.
i think the real issue isnt the pump its how we think about insulin like its some kind of magic fix. it just does what you tell it. if you dont know what you're doing itll just do it wrong. like a hammer. you dont blame the hammer when you hit your thumb.
Thank you for this comprehensive guide. It is imperative that individuals using insulin pumps adhere strictly to the protocols outlined. Regular site rotation, accurate carbohydrate counting, and vigilant monitoring are not merely recommendations-they are non-negotiable pillars of safe, effective therapy. I have personally witnessed the consequences of negligence, and I urge all users to treat this with the seriousness it demands.
This is all just corporate propaganda. Pump companies make billions off fear. You don’t need a pump. You just need to stop eating carbs. And why do they always say "check your tubing"? Because they know the tubing leaks. The whole system is designed to fail so you keep buying new parts. I’ve been off pumps for 7 years. My A1c is 5.8. No tech. Just food.
I find it irresponsible to recommend extended boluses for pizza. Fat delays digestion, yes-but encouraging people to manipulate insulin delivery for junk food is not diabetes management. It’s moral laziness. You should be eating real food, not engineering your pump to handle a cheeseburger.
pumps are cool i guess but honestly if you need this much tech to not die you might want to ask why your body hates you so much
This whole post is a scam. The FDA lets these devices through because Big Pharma owns them. You think they want you to be healthy? No. They want you to keep buying insulin, sensors, tubing, batteries. You’re a product. Wake up.
i used to think i was doing great until i started looking at my pump data. turns out i was giving myself 3x the insulin i needed at breakfast because i thought "more is better". then i crashed so hard i called 911. now i test my basal every 6 weeks. no more guessing. the pump doesn't lie. it just shows you how bad you are at math.
I just want to say how proud I am of everyone who’s learning to use a pump. It’s scary. I remember my first week-terrified to sleep, checking my screen every 20 minutes, convinced the pump was going to kill me. But you know what? I made it. And now I can go hiking, travel internationally, even have a glass of wine without panic. It’s not perfect, but it’s mine. And you’re doing better than you think. Keep going. You’ve got this.
I’ve been on a pump for 8 years and I still re-read this guide every few months. There’s always something I missed. Like the part about illness increasing insulin needs-last winter I got the flu and kept thinking I’d be fine if I just rested. Ended up in the ER. Now I have a sick-day protocol printed and taped to my fridge. Simple. But life-saving.
Excellent summary. I particularly appreciate the emphasis on backup insulin and glucagon. Too many people assume the pump is infallible. I once had a tubing kink during a flight-no alarms, no obvious signs. My blood sugar climbed to 18 mmol/L by the time I landed. Thank goodness I had my pen. Always carry backup. Always.