
It’s 2026. You walk into your pharmacy with a prescription for your blood pressure pill. The pharmacist hands you a small white bottle with a plain label. "This is the generic version," they say. "It’s the same active ingredient, but it costs $12 instead of $58." You stare at it. You’ve been taking the brand-name version for five years. You know how it works. You know how you feel on it. You’re not sure about this new bottle. This isn’t just you. It’s millions of people around the world. And it’s not because they’re irrational. It’s because brand loyalty in medications is deeply human - even when science says it doesn’t need to be.
Same pill, different price
The FDA and other global regulators require generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove they’re absorbed into the body at the same rate and to the same extent. In technical terms, they’re bioequivalent. That means, scientifically, they should work the same way. So why does a brand-name drug cost up to 79% more? And why do so many people still choose it? The answer isn’t in the chemistry. It’s in the mind.Trust isn’t built in labs - it’s built over time
Think about the first time you took a brand-name medication. Maybe it was for your child’s fever. Maybe it was after surgery. You trusted your doctor. You trusted the name on the bottle. You trusted the packaging. That first experience sticks. A 2023 study in the Indian Journal of Marketing found that brand experience is the strongest driver of loyalty for over-the-counter meds - even more than price or effectiveness. People don’t just trust the drug. They trust the story behind it. Brand-name companies spend years building that story. Ads on TV. Doctor visits. Patient support programs. Consistent packaging. Even the shape and color of the pill becomes part of the identity. When you see that familiar blue capsule, your brain associates it with relief. When you see a plain white tablet with a different shape, your brain doesn’t know what to do with it.Generics aren’t risky - but they feel risky
There’s a myth that generics are "inferior." They’re not. They’re held to the same strict standards. But perception doesn’t care about facts. Reddit threads like r/pharmacy are full of stories from people who say, "I tried three generics of my antidepressant. Only the brand worked." A 2022 Consumer Reports survey found 41% of people who switched to generics reported "noticeable differences" in effectiveness. The FDA says those differences are rare and usually due to placebo effects or unrelated changes in health. But that doesn’t matter to the person who felt worse. It’s not that generics are unsafe. It’s that people fear the unknown. Especially when it comes to mental health, chronic pain, or epilepsy. If a small change in dosage could mean a seizure, a panic attack, or a hospital visit, the brain chooses certainty - even if it costs more.Doctors aren’t immune either
You might think doctors are the ones pushing generics to save money. But they’re human too. A 2023 GlobalData survey found that 40% of physicians would prescribe brand-name drugs if cost weren’t an issue. In Japan, that number jumps to 57%. In Spain and Italy, it’s over 45%. Why? Some cite differences in regulatory standards. Others say they’ve seen patients struggle with generics in the past. Many just stick with what they know works.Age matters - and Gen Z is changing the game
Generational differences are stark. Millennials and Gen X are more likely to accept generics. But Gen Z? They’re the most loyal to brands - even when they’re 79% more expensive. A 2022 Fortune survey found 35% of Gen Z consumers prefer brand-name medications. Not because they’re wealthy. But because they’ve grown up in a world of branded experiences - Apple, Nike, Spotify. They don’t just buy products. They buy identity. Trust. Consistency. They’re not loyal because they’re naive. They’re loyal because they’ve learned that a brand that delivers on one thing - like a reliable phone or a smooth streaming app - will likely deliver on another, like a pill that doesn’t make them feel off.Who pays the price?
The cost isn’t just on your wallet. It’s on the whole system. In the U.S., generics make up 90% of prescriptions by volume. But they account for only 22% of total drug spending. That means brand-name drugs - just 10% of prescriptions - are taking 78% of the money. Pfizer, Johnson & Johnson, and AbbVie together took 18.7% of all U.S. prescription drug spending in 2022 - even after many of their patents expired. That money doesn’t vanish. It goes to marketing, lobbying, patient assistance programs, and shareholder returns. And it’s passed on to you through higher insurance premiums, higher taxes, and higher out-of-pocket costs.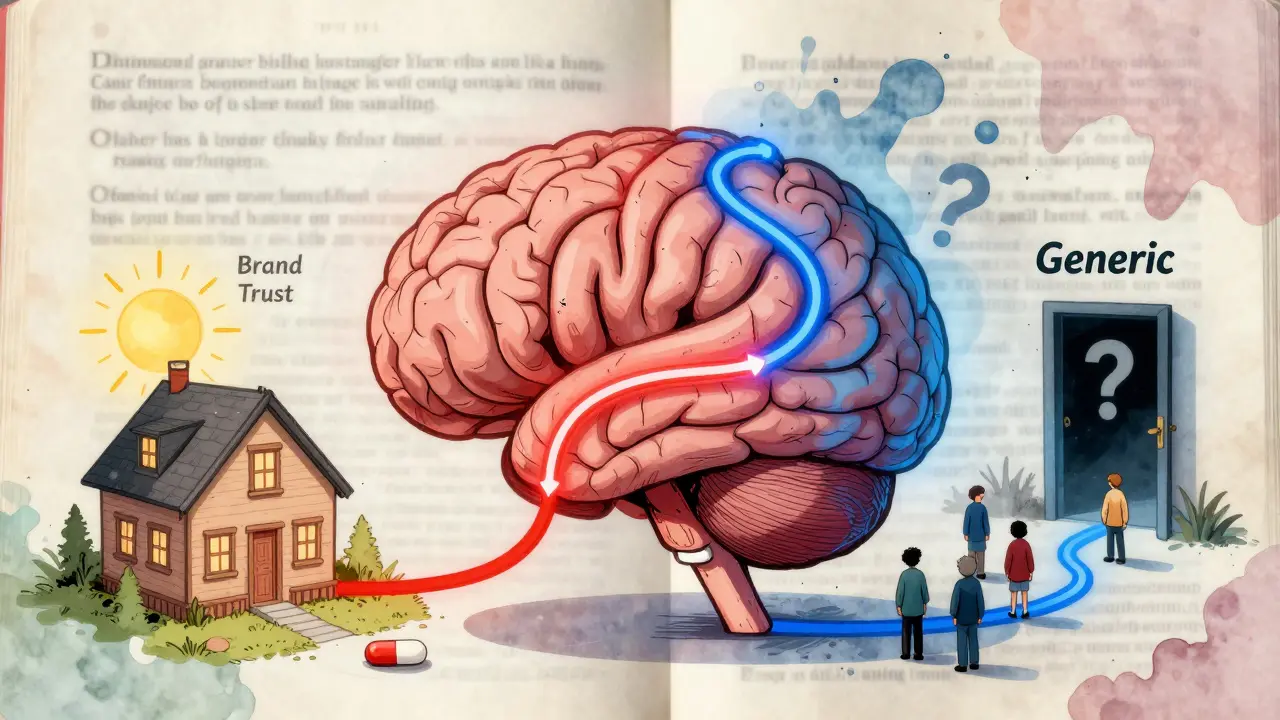
When brand loyalty saves lives - and when it doesn’t
There are real cases where brand loyalty matters. For complex biologics - like insulin, rheumatoid arthritis drugs, or cancer treatments - switching to a biosimilar (the generic version of a biologic) can cause anxiety. Only 32% of patients switch within the first year, even when it’s approved and cheaper. A 2023 study in the American Journal of Managed Care found 78% of patients are unwilling to switch. But for simple medications? Like statins, antibiotics, or antihistamines? Generic substitution rates are over 95%. No one’s afraid of a generic version of ibuprofen. Why? Because the stakes are lower. The body doesn’t notice tiny differences. And the cost difference is huge.How to make the switch - if you want to
You don’t have to stay loyal to a brand if it’s hurting your budget. Here’s how to make an informed choice:- Ask your pharmacist: "Is this generic rated "A" by the FDA?" That means it’s officially bioequivalent.
- Check the Orange Book online (FDA’s database of approved drugs) to confirm therapeutic equivalence.
- Don’t switch cold turkey. If you’re on a medication for anxiety, epilepsy, or heart disease, talk to your doctor first. They might suggest a trial period.
- Track how you feel. Keep a simple journal: sleep, energy, mood, side effects. Compare before and after.
- If you feel worse after switching, go back. Your experience matters more than any study.
The future is changing - slowly
The FDA’s new GDUFA III program aims to speed up generic approvals. Employers are pushing tiered copays - $5 for generics, $50 for brands. Insurance plans are refusing to cover brand-name drugs unless generics fail. But brand loyalty won’t disappear. It’s too deeply tied to trust, emotion, and fear. The companies that will survive aren’t the ones with the cheapest pills. They’re the ones who build relationships - patient support lines, apps that remind you to take your med, free samples, educational videos. In the end, medicine isn’t just chemistry. It’s psychology. And until we fix how we talk about generics - until we stop treating them like second-class options - brand loyalty will keep costing us billions.Maybe the real question isn’t why patients prefer brands. It’s why we haven’t made generics feel just as reliable.






10 Comments
Look, I get it - generics are technically the same. But if I take a pill that makes me feel like I’m slowly turning into a zombie, and then I switch to the brand and suddenly I’m not hallucinating my cat talking to me, that’s not placebo. That’s my nervous system screaming. Stop pretending science fixes everything when your brain is still wired to trust what’s familiar.
The data is clear: bioequivalence standards are rigorously enforced. The perceived differences are almost always psychological or due to concurrent health changes. Patients aren’t irrational - they’re responding to real anxiety about their health. The system needs better education, not more stigma against generics.
Bro, you think Americans are weird? In India, people pay 5x more for imported generics because the local ones look "too plain". We trust the color, the logo, the fancy bottle. If it doesn’t have a logo, it’s not medicine. Science? Nah. Branding is religion now.
Oh my god, I switched to a generic for my anxiety med… and I had a panic attack so bad I called 911… I swear to god I thought I was dying… and then I went back to the brand and I felt like I was hugged by a cloud… I don’t care what the FDA says… my soul knows the difference… please don’t tell me I’m wrong… I just want to feel safe…
My grandma takes the brand-name statin because the pill has a little groove on it that she says "feels right" in her hand. She’s 82. She’s not tech-savvy. She doesn’t care about cost. She cares about the ritual. And honestly? That ritual keeps her alive. Maybe we should stop trying to fix what’s working for people.
Let’s cut through the BS: brand-name companies don’t make better pills - they make better marketing. They fund patient advocacy groups, sponsor doctor conferences, and even design pill shapes to trigger dopamine hits. That blue capsule? That’s not medicine. That’s a dopamine trap. And Gen Z? They’re the first generation raised on branded experiences - they don’t buy products, they buy identity. So yeah, they’ll pay $58 for a pill that looks like an Apple product. It’s not stupidity. It’s capitalism.
It’s fascinating how we treat medication like a luxury brand - when in reality, it’s a lifeline. The fact that we’ve normalized paying 79% more for psychological comfort - while millions go without - is a moral failure disguised as consumer choice. Maybe instead of blaming patients, we should ask why we’ve made healthcare feel like a game of brand roulette.
I’ve been a pharmacist for 18 years. I’ve seen patients cry because they were forced to switch. I’ve also seen people save thousands by switching - and feel better than ever. The key isn’t forcing or shaming. It’s trust. If we could make generics feel like they have the same care behind them - same packaging, same support, same stories - people would switch. But right now? Generics feel like the hospital’s leftover food. They need a rebrand. Not the pill. The perception.
Okay but like… imagine if your Spotify Premium just got swapped for a random app that plays the same songs but the UI is ugly and the logo is a sad potato… you’d freak out right?? Same thing!! Brand = vibes!!
So we’ve reduced human trust to a pharmacokinetic equation? We’re so obsessed with the science that we forgot the soul. The pill doesn’t heal - the belief in the pill does. Maybe the real generic isn’t the drug… it’s the system that refuses to care about how people feel.