
Chloroquine Adherence Calculator
Treatment Adherence Calculator
Calculate your adherence rate and understand the risks of missed doses for chloroquine phosphate treatment
Your Adherence Assessment
Enter your treatment details above to see your adherence rate and risk assessment.
Imagine taking a life‑saving pill for weeks, only to stop halfway because you forget, feel side effects, or think you’re fine. That’s the reality for many people on chloroquine phosphate, and the gap between prescribed therapy and what patients actually do can mean the difference between cure and relapse.
What is Chloroquine phosphate?
Chloroquine phosphate is a synthetic antimalarial drug that has been used for decades to treat infections caused by Plasmodium parasites. It works by entering the parasite’s food vacuole, raising its pH, and blocking the detoxification of heme, which ultimately kills the parasite. Though newer drugs have taken the spotlight, chloroquine remains a cornerstone in many national malaria control programs, especially where resistance is still low.
Understanding patient adherence
Patient adherence refers to how well a person follows a prescribed medication schedule, including dose, timing, and duration. It’s not just about remembering to take a pill; it’s about staying on track even when life gets busy, side effects appear, or the benefits seem distant.
Why adherence is critical for malaria therapy
Malaria caused by Plasmodium falciparum is the deadliest form, responsible for most severe cases and deaths worldwide. A full therapeutic course of chloroquine phosphate eliminates blood-stage parasites, prevents recurrence, and reduces transmission. Skipping doses can leave a fraction of parasites alive, giving them a chance to multiply and potentially develop resistance.
Consequences of missed doses
- Treatment failure: Incomplete clearance leads to persistent fever, anemia, and organ damage.
- Resistance emergence: Sub‑therapeutic drug levels act like a training ground for parasites to adapt.
- Increased healthcare costs: Relapses often require hospitalization, additional diagnostics, and second‑line therapies.
- Community impact: Untreated carriers keep the transmission cycle alive, undermining public‑health campaigns.
Key factors that undermine adherence
Several real‑world issues push patients off track:
- Side effects: Nausea, itching, and visual disturbances can feel uncomfortable, prompting patients to stop early.
- Complex regimens: Some protocols require multiple daily doses over several days, increasing the chance of forgetfulness.
- Knowledge gaps: If patients don’t understand why the full course matters, they may stop once symptoms fade.
- Access barriers: Rural clinics might be far away, making follow‑up visits inconvenient.
- Cultural beliefs: Traditional remedies may be preferred over modern medicines in certain communities.
Evidence‑based strategies to boost adherence
Health programs worldwide have tested dozens of tactics. Below are the most successful, based on WHO guidelines and field trials.
Adherence‑boosting interventions Strategy How it works Typical impact on adherence Directly observed therapy (DOT) Healthcare worker watches each dose taken +30‑40% adherence Medication reminder apps Push notifications sync with dosing schedule +20‑25% adherence Simplified regimens Reduce daily doses, use fixed‑dose combinations +15‑20% adherence Patient education sessions Explain disease, drug action, and side‑effect management +10‑15% adherence Community health worker follow‑up Home visits for counseling and pill counts +12‑18% adherence
Practical tips for patients
- Keep the medication in a visible spot - like next to your toothbrush.
- Link each dose to a daily routine (breakfast, lunch, bedtime).
- Set an alarm on your phone or use a free reminder app.
- If side effects bother you, call your healthcare provider; they may adjust the schedule or offer supportive meds.
- Bring a pillbox to the clinic; the staff can pre‑fill it for you.
Monitoring adherence in clinical practice
Clinicians have several low‑cost tools:
- Pill counts: Ask patients to bring back empty blister packs.
- Self‑report questionnaires: Simple checklists that ask about missed doses.
- Blood level testing: Measuring chloroquine concentrations can confirm compliance, though it’s rarely used in low‑resource settings.
- Electronic dose‑recording devices: Smart caps log each opening, uploading data to a central server.
The best approach mixes objective checks (pill counts) with supportive conversation, avoiding a blame‑focused tone.

Case study: Rural clinic in Ghana
A government‑run health post introduced three changes in 2023: a weekly community‑health‑worker visit, a short animated video explaining why the full chloroquine course matters, and a free SMS reminder service. Over six months, adherence rose from 58% to 84%, while treatment failure dropped from 12% to 3%. The cost per additional adherent patient was less than $1, showing that simple, culturally tailored interventions pay off.
Bottom line
Chloroquine phosphate can cure malaria, but only when patients finish the entire regimen. Side effects, forgetfulness, and lack of understanding are the main hurdles. By pairing clear education, reminder tools, and community support, healthcare systems can dramatically improve adherence, protect patients, and keep resistance at bay.
Frequently Asked Questions
What is the standard dosage of chloroquine phosphate for uncomplicated malaria?
The typical adult regimen is 600mg base (equivalent to 1,000mg of chloroquine phosphate) loading dose on day1, followed by 300mg base (500mg phosphate) at 8h, 24h, and 48h. Exact dosing may vary with weight and local guidelines.
Can I use chloroquine phosphate to prevent malaria?
Yes, it is sometimes prescribed as chemoprophylaxis for travelers to low‑resistance areas, usually 300mg base weekly, starting one week before travel and continuing for four weeks after return.
What should I do if I experience itching after taking chloroquine?
Mild itching is a known side effect. Antihistamines like cetirizine can help. If the rash spreads or you develop fever, contact a clinician immediately.
How can I tell if I have missed a dose?
Check your pillbox or blister pack. If you’re unsure, take the missed dose as soon as you remember-unless it’s close to the next scheduled dose, in which case skip the missed one and continue as planned.
Is resistance to chloroquine still a problem?
In many parts of sub‑Saharan Africa, resistance has rebounded, making chloroquine less reliable. However, several islands in the Pacific and parts of South America still report low resistance, keeping the drug useful there.
Frequently Asked Questions
What is the standard dosage of chloroquine phosphate for uncomplicated malaria?
The typical adult regimen is 600mg base (equivalent to 1,000mg of chloroquine phosphate) loading dose on day1, followed by 300mg base (500mg phosphate) at 8h, 24h, and 48h. Exact dosing may vary with weight and local guidelines.
Can I use chloroquine phosphate to prevent malaria?
Yes, it is sometimes prescribed as chemoprophylaxis for travelers to low‑resistance areas, usually 300mg base weekly, starting one week before travel and continuing for four weeks after return.
What should I do if I experience itching after taking chloroquine?
Mild itching is a known side effect. Antihistamines like cetirizine can help. If the rash spreads or you develop fever, contact a clinician immediately.
How can I tell if I have missed a dose?
Check your pillbox or blister pack. If you’re unsure, take the missed dose as soon as you remember-unless it’s close to the next scheduled dose, in which case skip the missed one and continue as planned.
Is resistance to chloroquine still a problem?
In many parts of sub‑Saharan Africa, resistance has rebounded, making chloroquine less reliable. However, several islands in the Pacific and parts of South America still report low resistance, keeping the drug useful there.






13 Comments
Hey there thanks for sharing this info i really appreciate the effort you put into breaking down the adherence stuff it's super helpful and i kinda wish more people read it i think simple reminders like putting the pill next to your coffee mug can make a big difference let’s keep spreading the word
So you think this is just about “remembering to take a pill”? Wake up! The real agenda is hidden – big pharma pushes these meds while silencing the truth about natural immunity. They want us dependent, keep the population docile and the market booming. Don’t be fooled by glossy tables and official guidelines, they’re all part of the control machine.
Let me paint a picture for you: a mother in a remote village wakes up at dawn, her child feverish, the clinic a day’s trek away, the promise of a cure dangling like a fragile thread. She receives a blister pack of chloroquine, instructed to take it twice daily for three days, but life doesn’t pause for schedules. The first dose is taken with trembling hands, hope flickering in her eyes, yet the second dose is missed because the baby cries and the firewood runs out. By the third day she feels a slight improvement, the fever subsides, and she convinces herself that the battle is won. The remaining tablets gather dust, ignored, as the daily chores and worries consume her attention. Unbeknownst to her, a few parasites survived, lying in wait, their numbers quietly rebuilding under the surface of her bloodstream. When the fever returns, more vicious than before, the cycle repeats, each missed dose feeding the silent evolution of resistance. The community watches as treatment failures rise, the health workers scramble, and resources dwindle. In a desperate attempt, they intensify drug campaigns, but the parasites have already learned, adapting to the sub‑therapeutic levels left behind. The legacy of missed doses becomes a story of losses, both personal and public, etched into the collective memory of the village. Meanwhile, the data shows that a simple reminder-like a song on the radio or a chalkboard note-could have changed the outcome. Yet those quiet, low‑cost interventions are often overlooked in favor of expensive, high‑tech solutions that fail to reach the hands that need them most. The tragedy is not just that a life is at risk, but that the pattern repeats, a cascade of preventable relapses. Each forgotten pill becomes a brick in the wall of resistance, a barrier that future generations will have to climb over. So when we talk about adherence, we must see beyond the individual, recognizing it as a thread that weaves the health of entire communities, the stability of economies, and the very battle against a disease that has haunted humanity for millennia. Let’s invest in the small, human‑scale tools that keep people on track, because every dose taken is a step toward breaking this endless loop.
Interesting take, but let’s not forget the science is clear: adherence saves lives 😊. Skipping doses isn’t just a personal choice, it reshapes the parasite population and fuels resistance. The data from Ghana shows a jump from 58% to 84% when simple reminders were added – that’s a huge win. So before we spin conspiracies, consider the evidence and the real-world impact of sticking to the regimen. 🙃
Adherence matters.
The act of taking a pill is not merely a medical transaction; it is a ritual that binds the individual to the collective fate of humanity. When we neglect this ritual, we betray not only our own health but the fragile equilibrium of ecosystems that rely on us. The philosophy of duty compels us to honor the prescribed regimen, for neglect breeds chaos and invites the specter of resistance. Thus, each dose is a stanza in the grand poem of survival.
Totally agree – keep that pill routine tight and you’ll beat the bug. Small steps, big wins.
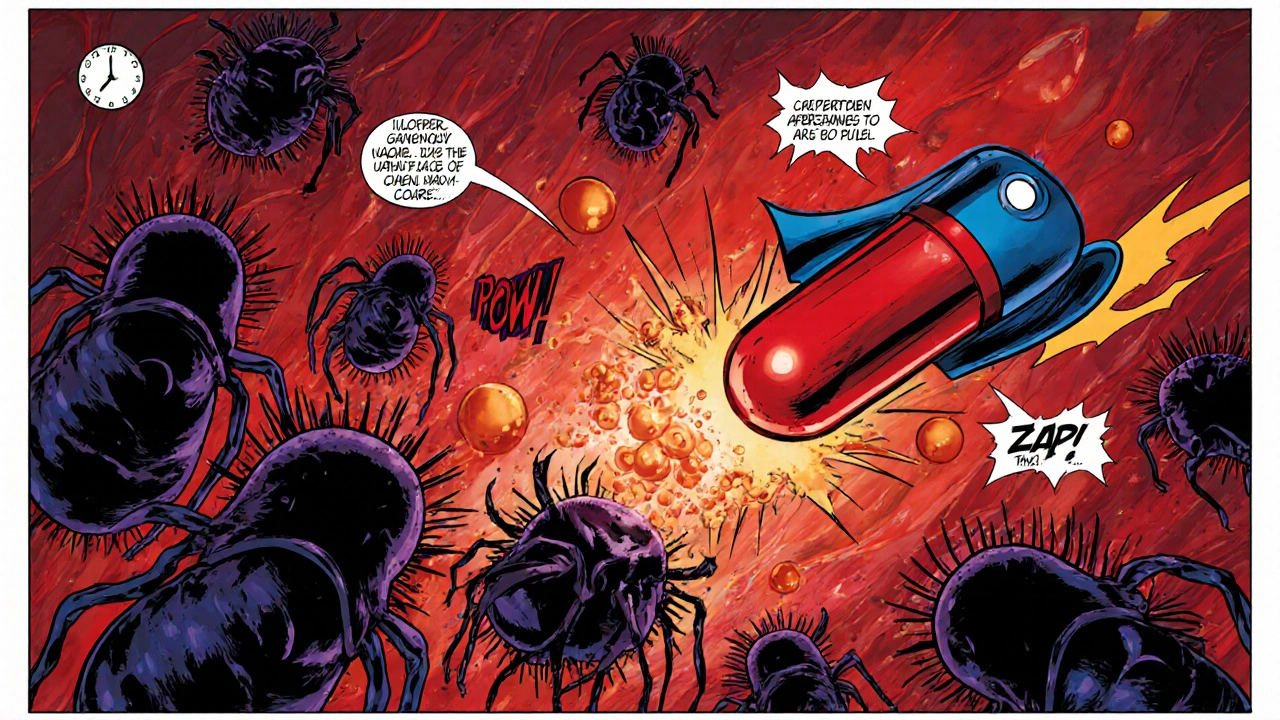
Think of the journey as a heroic quest. The malaria parasite is the dragon, and each dose of chloroquine is a sword strike. Miss a swing and the beast regains its strength, but stay relentless and you claim victory. Keep the rhythm, stay brave, and the story ends with you as the champion.
Sure, the “heroic quest” narrative is cute, but let’s not romanticize a drug that’s been weaponized by corporations. Real solutions lie in community empowerment, not just personal bravery.
pill reminder app is overkill just use alarm
Honestly, the simplest tools beat the fancy ones every time. 🚀 An alarm, a sticky note, a friend’s nudge – that’s all you need to stay on track. 🙌
Ugh, these guidelines are too long. Who has time to read all this? Just give us a one‑liner and we’re good.
Reading the details is essential; ignorance is the enemy of progress. In our nation’s interest, we must uphold rigorous standards and not reduce complex medical protocols to a mere slogan.