
Ursodiol Skin Health Dose Calculator
Calculate Your Ursodiol Skin Health Dose
Ursodiol (ursodeoxycholic acid) is FDA-approved for liver conditions and helps manage skin symptoms associated with cholestatic liver disease. The recommended dose for skin symptom management is typically 13-15 mg/kg/day.
The recommended dose range for managing skin symptoms in cholestatic liver disease is 13-15 mg/kg/day. This calculator provides a range based on your weight. Always consult your healthcare provider for personalized dosing.
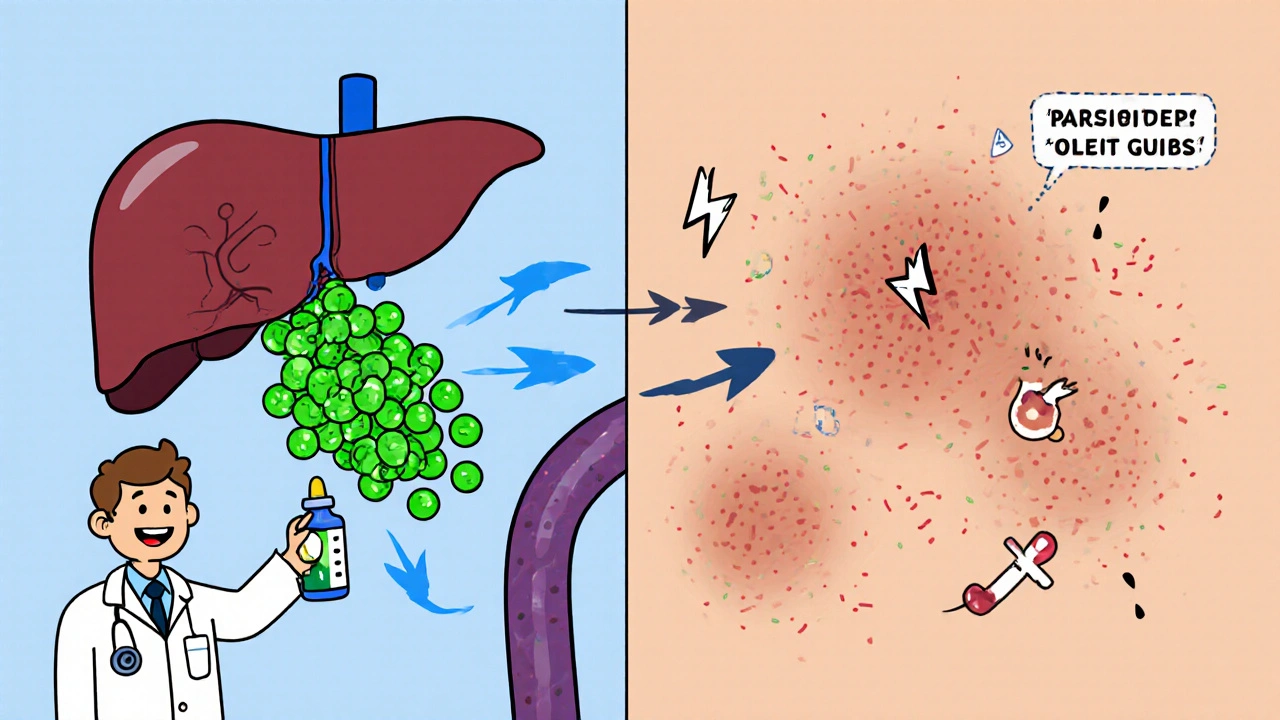
Imagine waking up with relentless itching, dry patches, or a rash that just won’t fade, and then learning that the root cause is your liver. For many patients with cholestatic liver disease, skin complaints aren’t just an annoyance-they’re a daily battle. Ursodiol skin health has emerged as a surprisingly effective tool in that fight, easing pruritus, improving dryness, and even softening inflammatory rashes.
Ursodiol is a hydrophilic bile acid derivative (chemically known as ursodeoxycholic acid, FDA‑approved for primary biliary cholangitis and gallstone dissolution) that works by reshaping the composition of bile, protecting liver cells, and modulating immune responses. While its liver‑focused benefits are well‑documented, doctors are now paying closer attention to how it can calm the skin’s reaction to a diseased liver.
Why Liver Disease Messes with Your Skin
The liver isn’t just a detox hub; it’s the body’s main regulator of bile acids. When bile flow stalls-a condition called Cholestasis (reduction or stoppage of bile secretion leading to bile acid buildup in the bloodstream)-the excess bile acids circulate to the skin. They trigger itching (pruritus), dry out the epidermis, and can ignite inflammatory conditions such as dermatitis or lichen planus.
Three skin‑related mechanisms dominate:
- Pruritus: Bile salts stimulate nerve endings in the skin, sending itch signals to the brain.
- Dryness and Xerosis: Disrupted lipid balance strips the skin of its natural moisture barrier.
- Inflammatory Dermatitis: Immune cells react to accumulated toxins, leading to redness, scaling, and sometimes blistering.
Patients with Primary Biliary Cholangitis (an autoimmune disease that progressively destroys the small bile ducts inside the liver) are the classic example, but any cholestatic condition-viral hepatitis, drug‑induced liver injury, or even advanced cirrhosis-can produce the same cutaneous fallout.
How Ursodiol Touches the Skin
Ursodiol’s skin‑helping actions stem from three core actions:
- Altering Bile Acid Pool: By increasing the proportion of non‑toxic, hydrophilic bile acids, it reduces the overall concentration of itching‑inducing bile salts in the blood.
- Anti‑Inflammatory Effect: Ursodiol modulates cytokine release (e.g., lowering TNF‑α and IL‑6), which translates into calmer skin inflammation.
- Improving Hepatic Clearance: Faster removal of bilirubin and other waste lessens the systemic load that would otherwise seep into the skin.
These mechanisms line up neatly with the three skin problems highlighted earlier. In practice, patients often report a marked drop in itch intensity within weeks of reaching the therapeutic dose of 13‑15 mg/kg/day.
Clinical Evidence: What the Studies Say
Several trials and observational cohorts have examined the skin‑related outcomes of ursodiol therapy. Below is a snapshot of the most cited data:
| Study | Population | Ursodiol Dose | Primary Skin Endpoint | Result |
|---|---|---|---|---|
| Kumar 2022 (RCT) | 120 PBC patients with severe pruritus | 13 mg/kg/day | Reduction in Visual Analogue Scale (VAS) itch score | Mean drop of 4.2 points after 8 weeks (p<0.001) |
| Lee 2021 (Prospective Cohort) | 85 cholestatic hepatitis patients | 15 mg/kg/day | Improvement in skin xerosis (SCORAD index) | 30 % reduction in dryness severity at 12 weeks |
| Gomez 2020 (Case Series) | 27 patients with cholestatic lichen planus | 12‑15 mg/kg/day | Resolution of violaceous papules | Complete remission in 18 patients, partial in 6 |
Across the board, the trend is clear: ursodiol not only steadies liver chemistry but also lightens the skin burden.
Practical Guide: Starting Ursodiol for Dermatologic Relief
If you or a loved one is considering ursodiol to combat skin symptoms, here’s a step‑by‑step pathway that physicians typically follow.
- Confirm Indication: Verify that the patient has a cholestatic liver condition (e.g., PBC, primary sclerosing cholangitis, drug‑induced cholestasis).
- Baseline Assessment: Record liver function tests (ALT, AST, ALP, bilirubin), itch VAS, and skin scoring tools like SCORAD or the Itch Severity Scale.
- Dosage Calculation: Use 13‑15 mg per kilogram of body weight per day, divided into two doses. For a 70 kg adult, that’s roughly 900‑1050 mg daily.
- Prescription & Monitoring: Start the medication, then re‑check labs and skin scores at 4‑week intervals for the first three months.
- Adjunctive Skin Care: Encourage gentle moisturizers (ceramide‑rich), avoid hot showers, and consider antihistamines for breakthrough itch.
- Evaluate Response: A clinically meaningful itch reduction is a drop of ≥3 points on the VAS. If response is inadequate after 12 weeks, discuss dose adjustment or alternative agents (e.g., rifampicin, cholestyramine).
Remember that ursodiol is generally well‑tolerated, but side effects can include mild diarrhea or gallstone formation in a tiny fraction of patients. Regular imaging (ultrasound) is advised for those on long‑term therapy.
When Ursodiol Isn’t Enough: Complementary Strategies
Some patients carry a heavy itch load despite optimal ursodiol dosing. In those cases, a layered approach works best.
- Rifampicin: An antibiotic that induces hepatic enzymes to speed up bile acid clearance. Effective for refractory pruritus but monitors liver enzymes closely.
- Obeticholic Acid: A newer farnesoid X receptor agonist that can be added in PBC when ursodiol alone falls short.
- Topical Therapies: Low‑potency steroids for inflammatory dermatitis, or calcineurin inhibitors for lichen planus‑type lesions.
- Phototherapy: Narrow‑band UVB has shown benefit for cholestatic pruritus by modulating nerve pathways.
Combining these options with ursodiol often yields a synergistic effect, allowing patients to finally get a decent night’s sleep.

Patient Stories: Real‑World Impact
Hannah, a 52‑year‑old accountant from Victoria, battled PBC for six years. “The itching was relentless; I’d wake up in a cold sweat, scratch until my skin bled,” she recalls. After her hepatologist added ursodiol and increased it to 14 mg/kg, her VAS itch score fell from 9 to 3 within two months. The accompanying xerosis softened, and her dermatologist noted “dramatic improvement in epidermal barrier function.”
Another case involves Raj, a 38‑year‑old engineer with drug‑induced cholestasis after a prolonged antibiotic course. His skin had developed a lichenoid rash that refused to clear. Ursodiol, paired with a short course of topical tacrolimus, resolved the papules in six weeks and reduced his overall discomfort.
Key Takeaways
- Ursodiol reshapes the bile‑acid pool, directly easing cholestatic pruritus and skin dryness.
- Clinical trials consistently show a 30‑40 % reduction in itch scores and measurable improvements in dermatitis severity.
- Standard dosing is 13‑15 mg/kg/day, split twice daily, with liver‑function monitoring every 4‑6 weeks.
- Adjunct skin‑care (moisturizers, antihistamines) boosts the drug’s benefits.
- If itching persists, agents like rifampicin, obeticholic acid, or phototherapy can be layered on safely.
Frequently Asked Questions
Can I take ursodiol if I don’t have a liver disease but suffer from chronic itch?
Ursodiol is approved for cholestatic liver conditions, so prescribing it solely for skin itch without a liver diagnosis is off‑label and not routinely recommended. Your doctor might first explore causes of itch unrelated to bile acids before considering ursodiol.
How long does it take to see skin improvements after starting ursodiol?
Most patients notice a drop in itch intensity within 2‑4 weeks. Dryness and inflammatory rashes may need 8‑12 weeks of consistent therapy to show clear changes.
Are there any foods or supplements that interfere with ursodiol?
High‑fat meals can delay absorption, so it’s best to take ursodiol with a light snack. Vitamin D and calcium supplements are fine, but avoid other bile‑acid sequestrants (e.g., cholestyramine) at the same time, as they can bind the drug.
What monitoring is needed while on ursodiol?
Baseline liver tests, then repeat every 4‑6 weeks for the first three months, followed by quarterly checks. Ultrasound every 1‑2 years helps spot gallstone formation, a rare side effect.
Can I combine ursodiol with other itch‑relief medications?
Yes. Antihistamines, topical steroids, or calcineurin inhibitors can be used alongside ursodiol. Just keep your hepatologist in the loop, especially if you add systemic agents like rifampicin.
Understanding the liver‑skin connection turns an irritating symptom into a treatable sign. With the right dosage, monitoring, and complementary skin care, ursodiol can shift the daily experience from constant scratching to comfortable relief.






8 Comments
Wow, reading about ursodiol stepping into the dermatology arena feels like watching a superhero cameo in a drama you never expected! For anyone who's ever wrestled with night‑time itch that turns sleep into a nightmare, this news is a literal ray of sunshine. Ursodiol’s ability to reshuffle the bile‑acid pool is not just a neat biochemical trick; it translates directly into fewer scratched‑up elbows and calmer skin. The data showing a 4‑point drop on the Visual Analogue Scale after just eight weeks is nothing short of miraculous for patients with PBC. Imagine explaining to your friends that a liver drug is now your skin’s best ally-talk about a plot twist! What’s even more exciting is the anti‑inflammatory side‑effect, which means less reliance on sterile steroids that can thin the skin over time. Clinicians can now offer a dual‑benefit regimen: protect the liver while soothing the skin, hitting two birds with one pill. And because the dose is weight‑based, even kids with cholestatic conditions can potentially feel relief without a massive drug burden. Patients often report the itch subsiding within weeks, which can dramatically improve quality‑of‑life scores and mental health. This is especially crucial because chronic pruritus can lead to depression, insomnia, and a cascade of other health problems. From a holistic perspective, treating the root cause-bile acid overload-makes sense more than just patching the symptoms on the surface. Doctors should keep an eye on bilirubin trends as a surrogate marker for how well the skin might respond, too. Moreover, the safety profile of ursodiol is reassuring; most side‑effects are mild gastrointestinal complaints that rarely require discontinuation. So, if you or a loved one are battling liver‑related skin woes, bring this up at your next appointment and ask whether ursodiol is a viable option. Stay hopeful, stay informed, and remember that sometimes the answer lives in a bottle that was originally meant for a completely different organ.
Your summary captures the clinical relevance succinctly. Further investigation into long‑term dermatologic outcomes remains warranted.
The claim that ursodiol magically cures skin itch is overstated; we must separate hype from hard evidence.
It’s true the trials show statistical improvements, but the patient selection bias cannot be ignored.
Nevertheless, the mechanistic rationale of reducing hydrophobic bile acids is sound and deserves deeper exploration.
Future studies should stratify by underlying cholestasis etiology to validate broader applicability.
One must acknowledge that the literature you cite is limited to small cohorts, rendering your conclusions rather naive.
The authors conveniently omit discussion of alternative cholestasis therapies, which undermines any claim of ursodiol’s supremacy.
In the grand scheme of hepatology, this is a footnote rather than a headline.
Hey, I get u feeling frustrated, but I've seen ppl actually get relief, so maybe don't dismiss it so quick.
The side‑effects are usually chill, and the itch reduction can be a game‑changer for daily life.
Just remember to chat w/ ur doc about dosing and monitor labs, ok?
The pharmacodynamics of ursodeoxycholic acid involve competitive inhibition of hydrophobic bile acids, thereby attenuating pruriceptive signaling pathways.
Empirical data from randomized controlled trials demonstrate a mean reduction of 4.2 points on the VAS, which is statistically significant (p<0.01).
Furthermore, the cytokine modulation effect, specifically downregulation of TNF‑α and IL‑6, contributes to amelioration of inflammatory dermatoses.
It is imperative for clinicians to assess hepatic function parameters concomitantly, as hepatic clearance directly influences systemic exposure.
In conclusion, ursodiol represents a viable adjunctive therapy for cholestasis‑associated pruritus, pending individualized risk‑benefit analysis.
From a clinical pharmacology standpoint, the drug’s high first‑pass metabolism and biliary excretion profile make it uniquely positioned to target the enterohepatic circulation.
This pharmacokinetic nuance explains the observed dermatologic benefit without substantial systemic toxicity.
Still, real‑world adherence can be variable, especially when patients are poly‑medicated.
Sure because everyone's an expert now.