Canagliflozin: What It Is, How It Works, and What You Need to Know
When you hear canagliflozin, a prescription medication used to treat type 2 diabetes by helping the kidneys remove excess sugar through urine. Also known as a SGLT2 inhibitor, it doesn’t just lower blood sugar—it changes how your body handles glucose entirely. Unlike insulin or metformin, canagliflozin works outside the pancreas and liver. It blocks a protein in your kidneys called SGLT2, which normally reabsorbs sugar back into your blood. When that block happens, sugar flows out with urine instead. Simple. Effective. And it doesn’t make you gain weight.
That’s why doctors are prescribing it more often—not just for blood sugar control, but because it lowers the risk of heart failure and slows kidney damage in people with type 2 diabetes. SGLT2 inhibitors, a class of diabetes drugs that include canagliflozin, dapagliflozin, and empagliflozin. Also known as gliflozins, they’ve changed how we think about treating diabetes. These aren’t just sugar-lowering pills—they’re protective tools. Studies show people on canagliflozin are less likely to be hospitalized for heart failure or need dialysis. That’s not a side effect. That’s the point.
But it’s not magic. You still need to drink enough water. Dehydration and low blood pressure are real risks, especially if you’re older or on diuretics. And while it helps your kidneys, it doesn’t fix damaged ones. If you already have kidney disease, your doctor will check your numbers closely before starting it. It also increases the chance of yeast infections—especially in women—because sugar in urine feeds yeast. Simple hygiene helps, but don’t ignore signs like itching or burning.
Canagliflozin doesn’t cause low blood sugar by itself. But if you’re taking it with insulin or sulfonylureas like glipizide, that risk goes up. That’s why drug interactions matter. You can’t just add it to your existing routine without talking to your provider. And if you’re planning surgery or are sick with an infection, your doctor might pause it temporarily. These aren’t warnings to scare you—they’re reminders that this drug works differently than others, and that’s both a strength and something to manage carefully.
People who’ve tried canagliflozin often say the biggest win is losing weight without trying. Some lose 5 to 10 pounds in the first few months—not because they’re eating less, but because their body is flushing out sugar. That’s a real benefit for someone with type 2 diabetes who’s been stuck in a cycle of weight gain and rising blood sugar. It also doesn’t require daily injections or complex dosing schedules. One pill a day, before breakfast, and you’re done.
But here’s the thing: it’s not for everyone. If you have severe kidney disease, it won’t work. If you’re prone to urinary tract infections, you might get more. And if you’re on a very low-carb diet, the risk of ketoacidosis—even with normal blood sugar—goes up. That’s rare, but it’s real. That’s why your doctor needs to know your full picture: your kidneys, your heart, your weight, your other meds.
Below, you’ll find real-world advice on how canagliflozin fits into diabetes care. You’ll see how it interacts with other drugs like metformin and insulin, why it’s used differently in older adults, and how it compares to other SGLT2 inhibitors. You’ll also find what to watch for when your body starts adjusting, and how to avoid common mistakes that lead to side effects. This isn’t theory. It’s what people are actually experiencing—and what doctors are learning from those experiences.
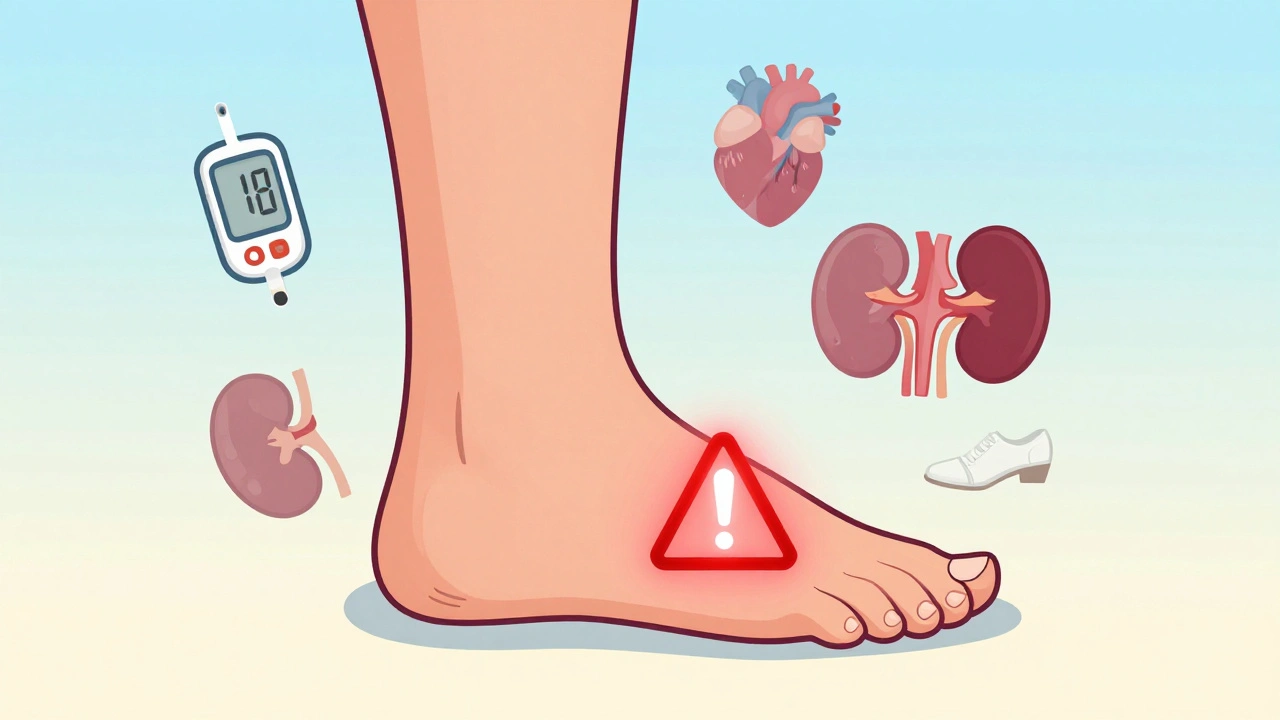
Canagliflozin and Amputation Risk: What You Need to Know Now
Canagliflozin increases the risk of foot and leg amputations in certain people with diabetes. Learn who’s at risk, how to prevent complications, and how this drug compares to other SGLT2 inhibitors like Jardiance and Farxiga.