Azathioprine and Allopurinol: Drug Interactions, Risks, and What You Need to Know
When you take azathioprine, an immunosuppressant used for autoimmune diseases and organ transplants. Also known as Imuran, it works by slowing down your immune system to prevent rejection or flare-ups. and allopurinol, a gout medication that lowers uric acid by blocking its production. Also known as Zyloprim, it’s one of the most common drugs for chronic gout. together, you’re walking into a hidden risk zone. This isn’t just a minor warning—it’s a potentially life-threatening interaction that many patients and even some doctors overlook.
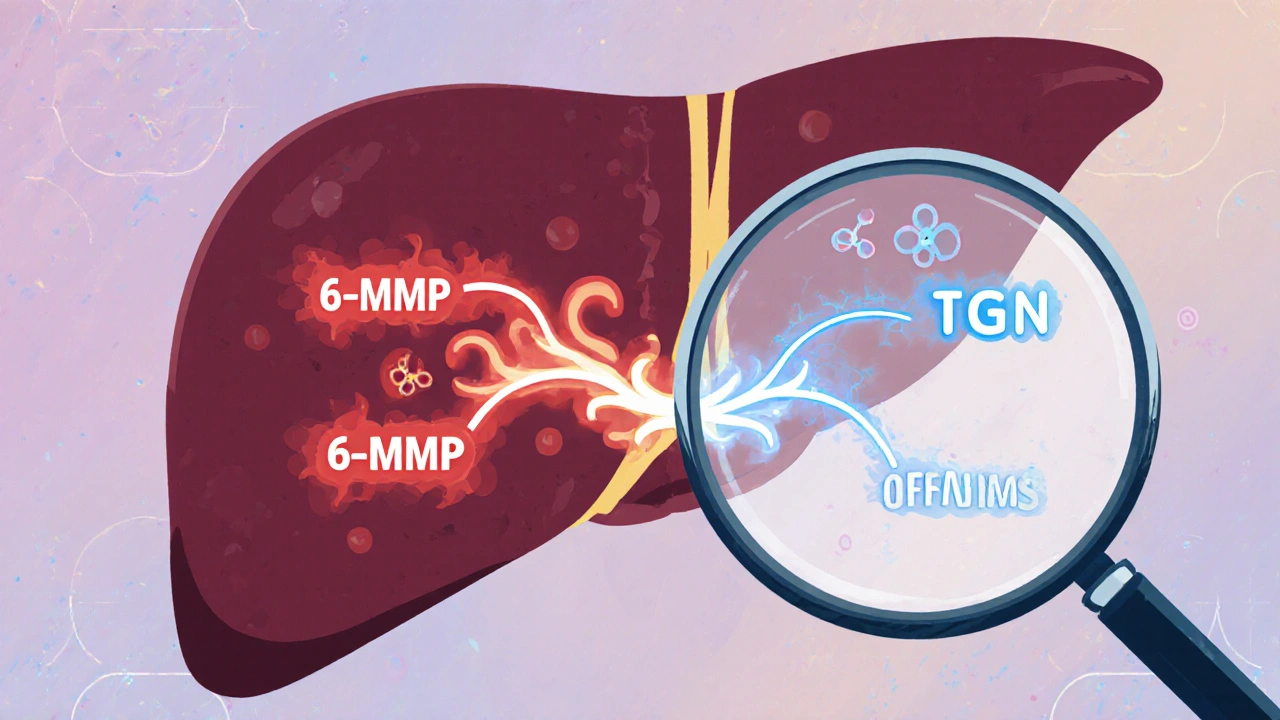
The problem starts in your liver. Azathioprine breaks down into active compounds called thiopurines, which your body clears using an enzyme called TPMT. Allopurinol doesn’t just lower uric acid—it also blocks another enzyme, xanthine oxidase, that helps break down those same thiopurines. When both drugs are in your system, thiopurines pile up like traffic on a closed highway. That buildup can crash your bone marrow, dropping your white blood cells, red blood cells, and platelets to dangerous levels. You won’t feel it right away. But weeks later, you might get a fever, feel exhausted, or notice unexplained bruising. By then, it’s already serious.
This interaction isn’t theoretical. Studies show that when allopurinol is added to azathioprine without adjusting the dose, the risk of severe bone marrow suppression jumps by up to 10 times. That’s why guidelines say: if you’re on azathioprine and need allopurinol, your azathioprine dose must be cut to 25% or less of what it was. Some doctors skip this step because they don’t realize how strong the effect is. Others assume the patient’s lab numbers are fine—until they’re not.
It’s not just about the two drugs. This interaction affects people differently based on genetics. Some people naturally have low TPMT enzyme activity—about 1 in 300 of us. For them, even normal doses of azathioprine can be risky. Add allopurinol, and the danger multiplies. That’s why some clinics test for TPMT before starting azathioprine. But not all do. And even if you’ve been on azathioprine for years without issue, adding allopurinol changes everything.
There are workarounds. Doctors might switch you to febuxostat, another gout drug that doesn’t interfere with thiopurine metabolism. Or they might monitor your blood counts weekly for the first month after adding allopurinol. But these steps only work if you and your doctor are aware of the risk. Too many patients are told, "It’s fine," when it’s not.
Below, you’ll find real-world posts that dig into this exact issue—along with related topics like drug metabolism, immune suppression, and how common medications like allopurinol can quietly disrupt other treatments. You’ll see how this interaction shows up in kidney disease, transplant care, and autoimmune conditions. You’ll also learn what to ask your doctor, what labs to track, and how to spot early warning signs before it’s too late. This isn’t just about two pills. It’s about understanding how your body handles them—and who’s really watching out for you.
Azathioprine and Allopurinol: How Low-Dose Combination Therapy Prevents Toxic Metabolite Buildup
LDAA therapy combines low-dose azathioprine with allopurinol to redirect toxic metabolite production, improving efficacy and reducing liver damage in IBD and autoimmune hepatitis patients with high TPMT activity.