6-MMP: What It Is, How It Affects Medications, and What You Need to Know
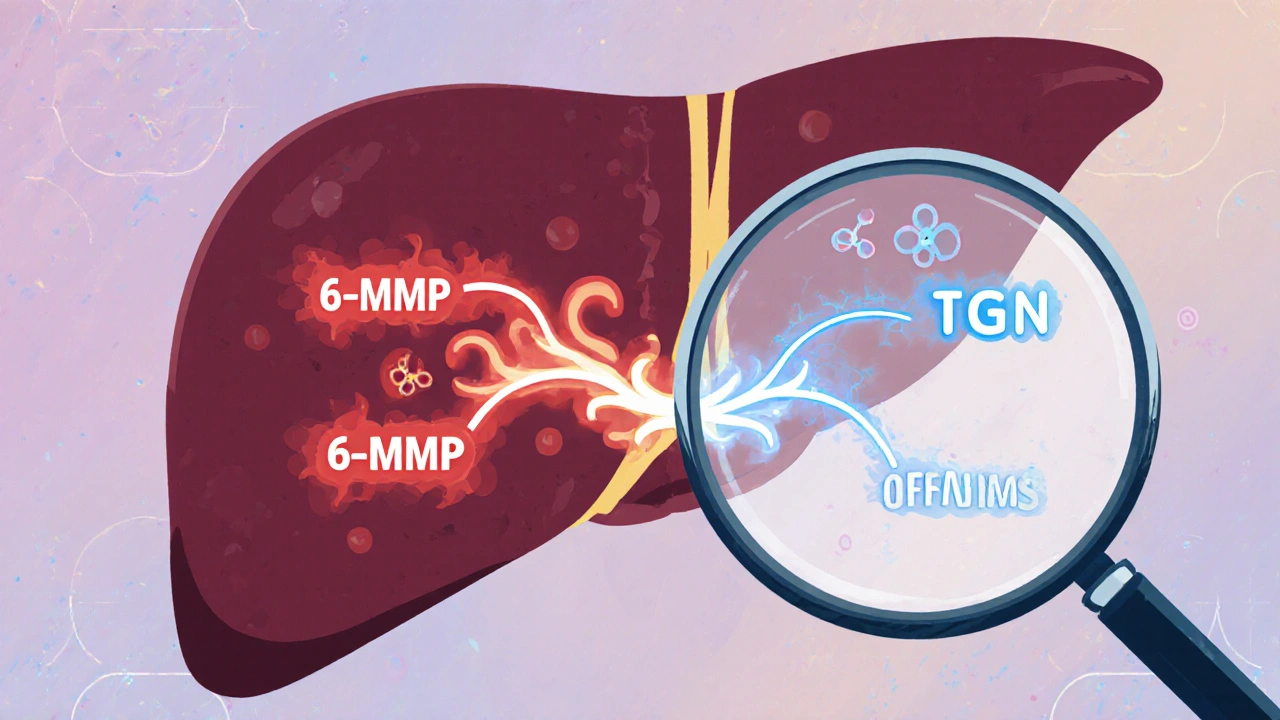
When your body breaks down medications, it doesn’t just flush them out—it transforms them. One of those transformations produces 6-MMP, a metabolite formed when the body processes thiopurine drugs like azathioprine and 6-mercaptopurine. Also known as 6-methylmercaptopurine, it’s not a drug itself, but it plays a huge role in how well those drugs work—and whether they cause harm. This isn’t just chemistry. It’s personal. If your body makes too much 6-MMP, you could be at risk for serious side effects. If it makes too little, the drug might not work at all.
What makes 6-MMP tricky is that it’s tied to another key player: CYP1A2, a liver enzyme that helps break down many drugs, including clozapine and some antidepressants. This enzyme doesn’t just handle one thing—it’s like a busy switchboard. Smoking, certain foods, and even other medications can turn CYP1A2 up or down. And when that happens, 6-MMP levels shift too. For someone on azathioprine for Crohn’s disease or leukemia, that shift can mean the difference between control and crisis. That’s why doctors sometimes test for 6-MMP levels directly. It’s not routine, but when a patient isn’t responding—or is getting sick from side effects—it’s one of the first things they look at.
And it’s not just about thiopurines. The same enzyme pathways that make 6-MMP also affect how drugs like clozapine, an antipsychotic used for treatment-resistant schizophrenia work. Smoking cuts clozapine levels by half, and that’s because CYP1A2 gets overworked. The same enzyme that clears clozapine also helps produce 6-MMP. So if you’re on both, your body is juggling two high-stakes processes at once. That’s why dose changes after quitting smoking aren’t optional—they’re life-saving.
You won’t find 6-MMP on most drug labels. But if you’re taking any thiopurine, or if you’re on meds that interact with CYP1A2, you need to know it exists. It’s the hidden link between your genes, your habits, and your treatment. Some people naturally make more 6-MMP because of their DNA. Others make more because they smoke, drink coffee, or take certain antibiotics. The result? One dose doesn’t fit all. That’s why personalized medicine isn’t a buzzword here—it’s a necessity.
Below, you’ll find real-world guides that connect the dots between 6-MMP, drug metabolism, and patient safety. From how smoking changes clozapine levels to why some people need different doses of azathioprine, these posts don’t just explain science—they show you what to do with it.
Azathioprine and Allopurinol: How Low-Dose Combination Therapy Prevents Toxic Metabolite Buildup
LDAA therapy combines low-dose azathioprine with allopurinol to redirect toxic metabolite production, improving efficacy and reducing liver damage in IBD and autoimmune hepatitis patients with high TPMT activity.