
When a rheumatologist prescribes Humira instead of a biosimilar, or an oncologist chooses Ocrevus over a cheaper alternative, it’s rarely about preference alone. It’s about survival, uncertainty, and a system that makes switching risky-even when the math doesn’t add up. Specialty drugs, which treat complex, life-altering conditions like multiple sclerosis, rheumatoid arthritis, and rare cancers, account for just 6.2% of all prescriptions in the U.S. But they consume 71.1% of total prescription drug spending. That’s not a typo. Less than 1 in 20 prescriptions drives more than 7 out of 10 dollars spent on meds.
Why Brand-Name Drugs Dominate Specialty Care
Specialty drugs aren’t like your typical pills you pick up at the corner pharmacy. They’re often injectables or infusions. Many require refrigeration, special handling, and ongoing monitoring. Some are given only through certified specialty pharmacies. And they’re expensive-often over $100,000 a year per patient. The average annual cost for a specialty drug user is $38,000. For non-specialty users? Just $492. That’s a 75-fold difference. So why do specialists keep reaching for the brand-name version? One reason is that many of these drugs have no real alternatives. Take Ocrevus for multiple sclerosis. While biosimilars exist, they’re not always interchangeable. A patient with a rare genetic mutation might respond to Ocrevus but not to anything else. The data isn’t there to prove safety or efficacy across all subgroups. So doctors play it safe. They prescribe what’s proven. A 2023 Medscape survey of 1,200 specialists found that 68% felt frustrated by prior authorization delays. Oncologists and rheumatologists were the most affected. One oncologist told me: “I spend 45 minutes on the phone with an insurer just to get approval for a drug my patient needs. If I switch to a cheaper option, I risk losing weeks-or months-of treatment time. That’s not worth the savings.”The Role of Fear and Uncertainty
Fear isn’t just emotional-it’s clinical. In oncology, for example, a single missed treatment window can mean the difference between remission and progression. Many specialty drugs were approved under accelerated pathways, meaning long-term data is still being collected. Switching to a biosimilar or generic might seem logical on paper, but in practice, it’s a gamble. A 2024 study in the Journal of Managed Care & Specialty Pharmacy found that 42% of specialty drug starts were delayed by more than seven days because of paperwork, insurance hurdles, or prior authorization. That delay isn’t just inconvenient-it’s dangerous. When a patient’s disease is actively progressing, time is the enemy. So if a brand-name drug is immediately available and covered, many specialists will choose it, even if a cheaper option exists. Patients themselves often push for brand names. A Reddit thread from November 2023 featured a patient with psoriasis who wrote: “My dermatologist says the biosimilar might work for most people, but I’ve had bad reactions to generics before. I’m not risking it.” That’s not irrational. It’s informed.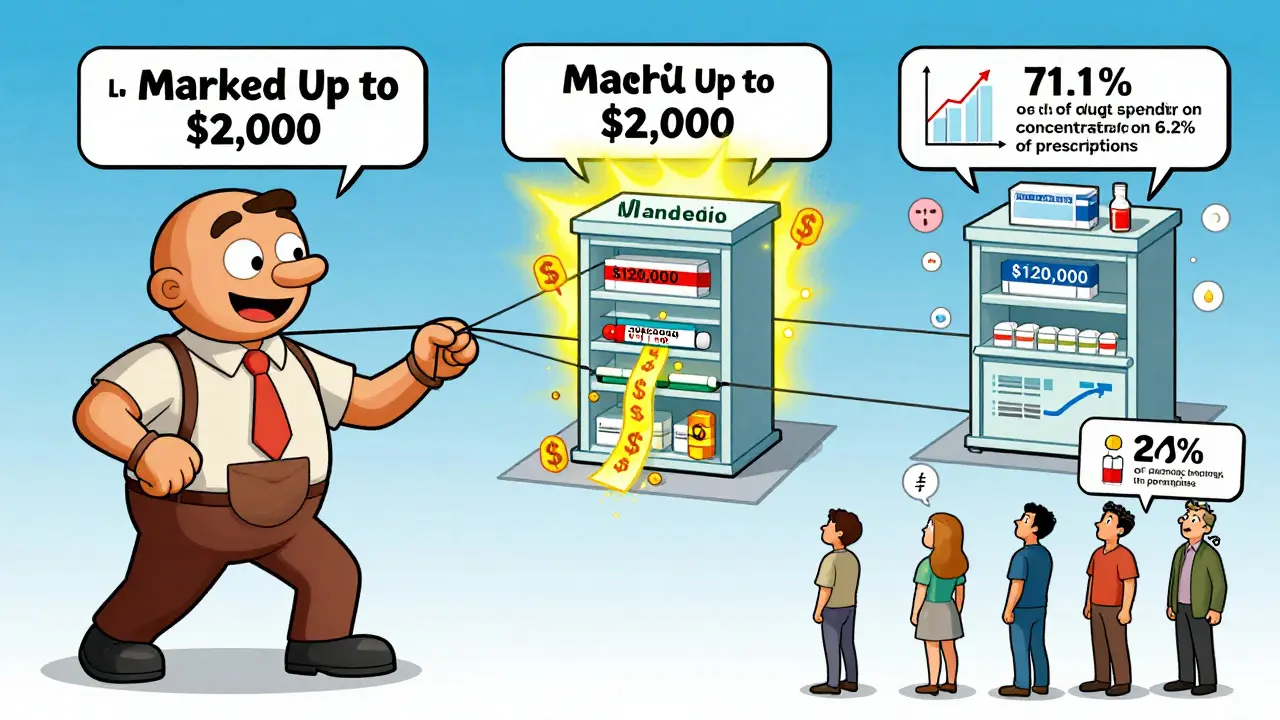
The PBM Problem
Behind the scenes, pharmacy benefit managers (PBMs)-the middlemen between insurers, pharmacies, and drugmakers-have created a system that rewards brand-name prescribing. The Federal Trade Commission’s January 2025 report found that PBMs marked up specialty generic drugs by thousands of percent. For example, a generic drug that costs $50 to acquire might be billed at $2,000. Meanwhile, brand-name drugs often come with rebates that PBMs keep, not pass on to patients or insurers. This creates a perverse incentive. If a PBM-owned pharmacy dispenses a brand-name drug, it gets a bigger cut than if it dispenses a generic. So even when a generic is available, the system pushes the more expensive option. This isn’t conspiracy-it’s business. And it’s working. The “Big 3” PBMs-Caremark, Express Scripts, and OptumRx-generated over $7.3 billion in revenue from dispensing drugs above their actual acquisition cost between 2017 and 2022.Industry Payments and Prescribing Patterns
It’s not just about PBMs. Drug companies spend billions on marketing directly to doctors. A ProPublica analysis from 2016 showed that physicians who received over $5,000 from pharmaceutical companies in 2014 prescribed brand-name drugs at a rate 50% higher than those who received nothing. Among internists, brand-prescribing rates jumped from 20% to 30%. This isn’t about corruption. It’s about influence. Free samples, educational dinners, speaker fees, and even travel reimbursements subtly shape prescribing habits. When a rep shows up with a patient assistance program for a $120,000-a-year drug, it’s easier to start there than to dig through formularies and prior auth forms for a cheaper alternative.
What’s Being Done?
Change is coming, but slowly. The Inflation Reduction Act of 2022 lets Medicare negotiate prices for some high-cost drugs-and several specialty drugs are already on the list. Drugs like Jakafi, Ofev, and Xtandi may soon be cheaper for Medicare patients. But this only affects one part of the system. Most specialty drug users are on private insurance. In March 2025, CMS proposed new rules requiring PBMs to disclose how much they’re marking up drugs. If implemented, this could force transparency. But will it change behavior? Probably not overnight. Meanwhile, patient assistance programs are filling gaps. In 2023, the National Organization of Rare Disorders helped 45,000 people access specialty drugs they couldn’t afford. But that’s a Band-Aid. It doesn’t fix the system.Where Do We Go From Here?
Specialists aren’t blindly choosing brand-name drugs because they’re greedy. They’re choosing them because the system makes it easier, safer, and sometimes the only viable option. The problem isn’t the doctors-it’s the structure. Real reform needs three things:- Transparency: PBMs must disclose their markups and rebates.
- Streamlined Access: Prior authorization should be automated, not a 45-minute phone call.
- Real Data: We need long-term studies comparing biosimilars and generics to brand-name drugs in real-world patient populations-not just clinical trials.
Why do specialists prefer brand-name drugs over generics in specialty care?
Specialists often choose brand-name drugs because many specialty conditions have no proven alternatives. Biosimilars and generics may lack long-term data for rare patient subgroups, and switching can risk treatment delays or adverse reactions. Additionally, prior authorization hurdles make switching slow and unreliable, while PBMs often incentivize brand-name prescribing through hidden rebates and markups.
Are brand-name specialty drugs really more effective than generics?
For many specialty drugs, especially biologics, there’s no clinical proof that generics or biosimilars are equivalent across all patient types. While they’re designed to be similar, real-world responses vary-especially in patients with rare mutations or complex immune profiles. Doctors avoid switching not because they distrust generics, but because the data isn’t there to guarantee safety for every individual.
How do pharmacy benefit managers (PBMs) influence brand-name prescribing?
PBMs profit more from brand-name drugs because they receive rebates from manufacturers and often mark up specialty generics by thousands of percent. For example, a generic drug costing $50 to buy might be billed at $2,000. PBMs also own specialty pharmacies, creating a conflict of interest: they make more money pushing expensive brands than cheaper alternatives, even when clinical guidelines support switching.
Do pharmaceutical companies influence doctors’ prescribing habits?
Yes. Studies show doctors who receive payments or gifts from drug companies prescribe brand-name drugs at significantly higher rates. One ProPublica analysis found physicians receiving over $5,000 from pharma companies prescribed brands 50% more often than those who received nothing. While not illegal, these interactions subtly shape decisions-especially when brand reps offer free samples or patient assistance programs.
What’s being done to lower specialty drug costs?
The Inflation Reduction Act allows Medicare to negotiate prices for some high-cost specialty drugs, starting with medications like Jakafi and Ofev. CMS also proposed new rules in March 2025 requiring PBMs to disclose their markups. But these changes affect only Medicare and don’t fix the broader system. Patient assistance programs help individuals, but they’re not a systemic solution.
Why do prior authorizations delay specialty drug prescriptions?
Prior authorizations for specialty drugs are often manual, requiring doctors to submit lengthy paperwork, call insurers, and wait days for approval. A 2023 Medscape survey found 68% of specialists face frequent delays, with oncologists and rheumatologists hit hardest. These delays can push treatment back by weeks-time patients with aggressive diseases can’t afford.






9 Comments
so basically doctors are just pawns in a game where the real winners are the guys in suits who don't even know what a cytokine is. brilliant.
Ah yes, the classic American healthcare opera-where the aria is sung by PBMs in tailored suits and the chorus is made up of physicians exhausted from filling out Form 7B-Alpha. Truly, Shakespearean in its tragedy. And yet, we still act surprised when the patient dies.
The structural inefficiencies in the specialty drug supply chain are a textbook case of principal-agent misalignment. PBMs act as third-party intermediaries with opaque rebate structures that distort incentive compatibility. Meanwhile, clinical decision-making is constrained by administrative burden, leading to suboptimal therapeutic trajectories.
You know what’s wild? The same people who scream about "big pharma" never mention that the real money is in the middle-PBMs, insurers, pharmacy chains. Doctors? They’re just trying not to kill their patients while the system laughs all the way to the bank. And we wonder why trust in medicine is collapsing.
I've been in this game for 20 years and let me tell you, it's not the doctors. It's the damn forms. You spend more time on the phone with an insurer than you do with the patient. And when you finally get approval? The patient's condition has worsened. So yeah, you stick with the brand. Because you're not just a doctor-you're a damn survivalist in a war zone with paperwork as the enemy. And don't even get me started on the 'biosimilars'-half the time they're not even tested on people like mine. You think I wanna gamble with someone's life? No. I wanna go home at night without another nightmare.
I work in a specialty pharmacy. I see the letters. The appeals. The tears. One patient cried because her insurance wouldn't cover the Humira until she tried three cheaper drugs-each one made her worse. She was 28. She had a 2-year-old. The system didn't care. The doctor did. So he prescribed anyway. And we filled it. Because sometimes, doing the right thing means breaking the rules.
The problem isn't the drugs. It's the middlemen. PBMs are the real parasites. They're not even in the business of health. They're in the business of profit extraction. And the worst part? No one talks about it because the media only cares about drug prices, not the hidden fees that double them.
This is why I became a pharmacist. To help people, not play accounting games. 💔 I’ve had patients cry in my office because they couldn’t afford their meds-even though they had insurance. I’ve seen doctors cry too. We’re not the enemy. The system is. And if we don’t fix the incentives, we’re just rearranging deck chairs on the Titanic. 🚢
Let’s be real: this isn’t about healthcare. It’s about capitalism with a stethoscope. We’ve turned human suffering into a spreadsheet. A $120,000 drug isn’t expensive because it’s hard to make-it’s expensive because someone figured out how to monetize desperation. And guess what? The people who benefit the most? They don’t have MS. They don’t have cancer. They don’t have psoriasis. They have a corner office and a private jet. And they’re still wondering why people are angry. The tragedy isn’t the cost of the drug. It’s that we’ve accepted this as normal. We’ve normalized the exploitation of the sick. And that’s not just broken. That’s evil.