When you’re managing diabetes, taking the right medication is only half the battle. The real danger often comes from what you’re taking with it. Many people don’t realize that common drugs - from antibiotics to blood pressure pills - can throw your blood sugar into chaos. One wrong combo can send you into a dangerous low, or push your glucose sky-high without warning. These aren’t rare edge cases. They happen every day, often because the patient or even the doctor didn’t check for interactions.
Why Some Diabetes Drugs Play Nicely - and Others Don’t
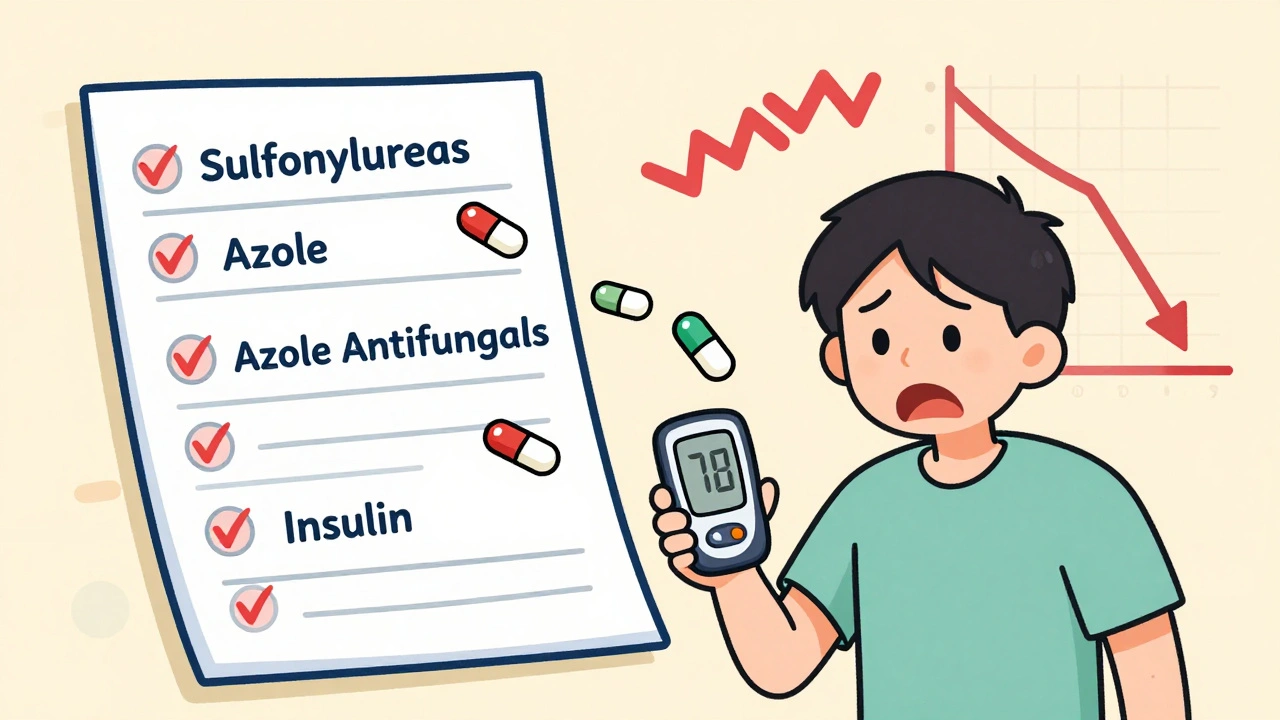
Not all diabetes medications interact the same way. Older drugs like sulfonylureas (glyburide, glipizide) and meglitinides (repaglinide, nateglinide) are the most trouble-prone. They work by forcing your pancreas to pump out more insulin. That’s great for lowering blood sugar - until something else boosts that effect too much. That’s when hypoglycemia hits hard, fast, and sometimes without warning. Newer drugs like GLP-1 receptor agonists (semaglutide, liraglutide) and SGLT-2 inhibitors (empagliflozin, dapagliflozin) are much safer in combination. They don’t force insulin release. Instead, they help your body use insulin better or flush out sugar through urine. That’s why they’re now often the first choice when adding a second drug to metformin.The Top 5 Dangerous Combinations You Need to Know
- Insulin + Rosiglitazone - This combo used to be common, but it’s now strongly discouraged. Rosiglitazone causes fluid retention, and insulin makes it worse. Together, they can trigger sudden heart failure or severe swelling in the legs and lungs. Even patients with no prior heart issues are at risk.
- Meglitinides + Azole Antifungals (ketoconazole, itraconazole) - These antifungals block the liver enzymes (CYP3A4 and CYP2C8) that break down repaglinide and nateglinide. The result? Drug levels build up in your blood, causing prolonged, life-threatening lows. One study showed blood sugar dropping below 40 mg/dL within hours of taking fluconazole with repaglinide.
- Metformin + Contrast Dye (for CT scans) - Metformin is cleared by the kidneys. Contrast dye can temporarily wreck kidney function. If you take metformin right before or after a scan, you risk lactic acidosis - a rare but deadly buildup of acid in the blood. Always stop metformin 48 hours before any contrast imaging, and only restart after your kidneys are checked.
- Insulin or Sulfonylureas + Quinine (for leg cramps) - Quinine, found in some over-the-counter cramp remedies and even tonic water, can trigger severe hypoglycemia. It’s not just a theory - emergency rooms see cases every year from people who thought tonic water was harmless.
- DPP-4 Inhibitors + GLP-1 RAs - These two drug classes work on the same pathway. Taking both (like sitagliptin with semaglutide) doesn’t give you better control - it just increases side effects like nausea and pancreatitis risk. The American Diabetes Association explicitly says this combo is unnecessary and should be avoided.
Drugs That Hide in Plain Sight
You might not think of these as diabetes killers, but they’re sneaky:- Corticosteroids - Prednisone, dexamethasone - even a short course for allergies or inflammation can spike your glucose for days. If you’re on insulin or sulfonylureas, you may need a temporary dose increase. Never ignore this - it’s one of the most common reasons people end up in the ER with diabetic ketoacidosis.
- Diuretics (water pills) - Hydrochlorothiazide and furosemide can raise blood sugar by reducing insulin sensitivity. If you’re on these for high blood pressure, your diabetes meds might need adjusting.
- Somatostatin analogues (octreotide) - Used for certain tumors or severe diarrhea, these drugs can flip-flop your blood sugar. They might cause low blood sugar at first, then high blood sugar later. Monitoring is critical - sometimes hourly.

How to Protect Yourself
You don’t need to memorize every interaction. But you do need a system:- Keep a full list - Write down every pill, patch, injection, and supplement you take. Include over-the-counter meds and herbal teas. Bring this list to every appointment.
- Ask your pharmacist - When a new drug is prescribed, ask: “Could this affect my diabetes meds?” Pharmacists are trained to catch these combos. Many will flag it before you even leave the counter.
- Test more often - If you start a new medication, check your blood sugar 2-4 times a day for the first week. Look for patterns. A drop at 2 p.m. every day? That’s not coincidence.
- Know your warning signs - Shaking, sweating, confusion, rapid heartbeat - these are low blood sugar signs. But if you’re on certain meds like beta-blockers, those symptoms can disappear. If you feel off, test - don’t wait.
What’s Safer Now? The New Rules for Combining Drugs
The 2025 American Diabetes Association guidelines have shifted. The old model - add a pill, then another, then insulin - is outdated. Now, the preferred path looks like this:- Start with metformin - it’s still first-line, low-cost, and low-risk for interactions.
- Add a GLP-1 RA if you need more control - they help with weight loss and have minimal interaction risk.
- If you still need more, add an SGLT-2 inhibitor - they reduce heart and kidney risks too.
- Only add insulin if the above aren’t enough - and even then, pair it with a GLP-1 RA. Studies show this combo lowers hypoglycemia risk by 30% compared to insulin alone.

What About Supplements?
People think “natural” means safe. It doesn’t. Here’s what to watch for:- St. John’s Wort - Speeds up liver metabolism. Can make metformin, sulfonylureas, and even insulin less effective.
- Chromium - May lower blood sugar. Can cause lows if taken with insulin or sulfonylureas.
- Alpha-lipoic acid - Often used for nerve pain. Can enhance insulin sensitivity - again, risk of hypoglycemia.
When in Doubt, Test
There’s no substitute for real-time data. Technology makes monitoring easier than ever. Continuous glucose monitors (CGMs) are now widely covered by insurance. If you’re on multiple diabetes drugs or starting a new medication, a CGM can show you exactly what’s happening - not just at fasting, but after meals, after exercise, even at night. One patient in Perth, on repaglinide and a new antibiotic, noticed her CGM spiked at 3 a.m. every night. She didn’t feel symptoms. But the graph showed a dangerous dip followed by a rebound. Her doctor switched the antibiotic, and her numbers stabilized within days.Final Thought: It’s Not About Avoiding Meds - It’s About Managing Risk
You need your diabetes medications. The goal isn’t to stop them. It’s to use them wisely. The right combinations can give you better control, fewer complications, and more energy. The wrong ones? They can land you in the hospital. Stay informed. Stay vigilant. And never assume a new pill is safe just because it’s for something else.Can I take antibiotics while on diabetes medication?
Some antibiotics can dangerously lower blood sugar when taken with sulfonylureas or meglitinides. Azole antifungals like ketoconazole and certain macrolides like clarithromycin are especially risky. Always tell your doctor you have diabetes before starting any antibiotic. They can choose a safer option or adjust your diabetes dose.
Does metformin interact with blood pressure meds?
Most blood pressure medications are safe with metformin. But thiazide diuretics (like hydrochlorothiazide) can raise blood sugar, making metformin less effective. Beta-blockers can mask the symptoms of low blood sugar, making it harder to recognize when you’re in danger. Monitor your glucose closely if you start or change a blood pressure drug.
Why is insulin combined with GLP-1 RAs better than insulin alone?
Combining insulin with a GLP-1 receptor agonist like semaglutide gives you better blood sugar control with less weight gain and fewer low-blood-sugar episodes. GLP-1 RAs slow digestion, reduce appetite, and help your body use insulin more efficiently. This means you often need less insulin, lowering your risk of hypoglycemia. Studies show a 30% drop in severe lows compared to insulin-only regimens.
Can I drink alcohol with my diabetes meds?
Alcohol can cause low blood sugar, especially when combined with insulin or sulfonylureas. It blocks the liver from releasing glucose, which is your body’s safety net during a low. If you drink, do so with food, never on an empty stomach. Limit to one drink per day and check your blood sugar before bed. If you use an insulin pump or CGM, set an alert for overnight lows.
What should I do if I accidentally take a dangerous combo?
If you take a drug that interacts with your diabetes medication, check your blood sugar immediately. If it’s low, treat it with fast-acting sugar (glucose tabs, juice). If it’s high, check for ketones if you’re on insulin. Call your doctor or go to urgent care if you feel confused, dizzy, or have chest pain. Don’t wait - some interactions can turn dangerous within hours.






15 Comments
Just had to share this - I started using a CGM last year after my doc flagged me for frequent lows. I didn’t even know I was dropping at night until the graph showed it. That post nailed it - real-time data is the game changer. No more guessing. I wish I’d known this five years ago.
GLP-1 RAs + SGLT-2 inhibitors as first-line combo after metformin? That’s the new standard of care. The EMPA-REG and LEADER trials showed mortality benefits beyond glucose control. If your doc’s still pushing sulfonylureas as first add-on, they’re operating on 2010 guidelines.
Let’s be real - the FDA’s approval process is a joke. They greenlight drugs like rosiglitazone knowing the cardiac risks, then act shocked when people die. This isn’t about patient education - it’s about pharma lobbying and profit margins. The system is rigged, and we’re the collateral damage.
St. John’s Wort? Please. I’ve seen people take it with metformin and wonder why their A1C jumped 2 points. It’s not ‘natural’ - it’s a potent CYP3A4 inducer. Same with grapefruit juice - it’s not just for statins. It wrecks metformin clearance too. If you’re on diabetes meds, avoid anything labeled ‘herbal remedy’ unless your endo vouched for it.
So you’re telling me I can’t have my tonic water with lime anymore? I mean, I know it’s sugar-free, but now I’m supposed to believe quinine’s the silent killer? Next they’ll say aspirin causes diabetes. This is just fearmongering dressed up as medical advice. I’ll take my gin and tonic and my A1C of 6.2, thank you very much.
It is both a moral and epistemological imperative that patients assume responsibility for their own pharmacological safety. The onus lies not upon the physician - who is constrained by time, systemic inefficiencies, and incomplete data - but upon the individual who ingests the substances. One cannot outsource agency to a medical professional and then lament the consequences of ignorance. This is not merely a clinical issue - it is a failure of personal sovereignty.
I’ve been on metformin and Januvia for six years. Last month my doc added a new blood pressure med - losartan. No big deal, right? Wrong. I started crashing at 3 a.m. every night. I thought I was just stressed. Then I checked my CGM - 48 mg/dL. No shaking, no sweating. Just… foggy. I almost passed out getting up to pee. I called my pharmacist. They said losartan doesn’t usually interact, but beta-blockers do. I wasn’t on a beta-blocker. Then I remembered - I’d been taking melatonin for sleep. Turns out melatonin can amplify insulin sensitivity. My doc switched me to magnesium glycinate. No more lows. I didn’t even know melatonin could do that. People need to stop assuming supplements are safe. They’re drugs. Just unregulated ones.
They say ‘test more often’ like it’s that easy. I work two jobs. I have three kids. I don’t have time to poke my finger every two hours. And don’t get me started on the cost of CGMs - insurance denies them unless you’re on insulin and have HbA1c over 9. That’s not prevention - that’s punishment for being poor. This whole system is designed to make you suffer before they’ll help you. And now they want me to ‘stay vigilant’? Yeah, right. I’m just trying to survive.
Big thanks for the breakdown on DPP-4 + GLP-1 RAs. I’ve seen that combo prescribed before - it’s pointless. You’re doubling side effects for zero benefit. Also - corticosteroids? I had a flare-up of my eczema last winter and got a 5-day prednisone pack. My sugars went from 140 to 320 overnight. I had to double my basal insulin. My endo didn’t warn me. I had to Google it myself. Always assume any new med - even a short course - will mess with your glucose. Test. Test. Test.
My grandma took repaglinide and got a prescription for fluconazole for a yeast infection. She ended up in the ER with a blood sugar of 32. She didn’t even know what she was taking. No one asked her about her diabetes meds. This is why pharmacists need to be the frontline defense. If your pharmacy doesn’t flag interactions automatically, switch pharmacies. It’s not optional.
Medicine is a religion. The gods are the FDA and Big Pharma. We are the faithful. We bow to pills. We forget our bodies know how to heal. The real cure is diet, movement, sleep. But no one wants to talk about that. Too simple. Too expensive to sell.
Let’s be honest - if you’re still on sulfonylureas, you’re not getting the best care. You’re getting the cheapest care. GLP-1s cost more? So does a heart attack. So does dialysis. So does an amputation. The real cost isn’t the pill - it’s the consequence of inaction. Stop being cheap. Your life isn’t a budget spreadsheet.
One thing I’ve learned after 12 years with type 2 - no one knows your body like you do. If something feels off after a new med, trust that. Even if your doctor says it’s fine. Keep a log. Note the time, the food, the stress, the sleep. Patterns reveal truths. I caught a hidden interaction between my thyroid med and metformin because I tracked it for three weeks. No one told me to. I just knew something wasn’t right.
Pharmacists are unsung heroes. I’ve had them catch interactions my doctor missed. Always ask. Always bring your list. Always read the insert. Even if it’s 12 pages long. Knowledge is not optional. It is your right. And your responsibility.
Did you know the FDA approved metformin in 1994 but didn’t require interaction studies until 2010? That’s 16 years of people getting hurt. And now they want us to trust the system? They’re still approving drugs that cause pancreatitis. They’re still allowing contrast dye without kidney checks. This isn’t medical advice - it’s corporate damage control. They want you to think you’re safe. You’re not.