
Every year, Americans spend over $650 billion on prescription drugs. That’s more than any other country in the world. But here’s the surprising part: generics make up 90% of all prescriptions filled - yet they account for just 12% of total spending. Meanwhile, brand-name drugs, which make up only 10% of prescriptions, swallow up 88% of the bill. This isn’t magic. It’s economics. And it’s working.
What Exactly Are Generic Drugs?
Generic drugs aren’t cheap knockoffs. They’re exact copies of brand-name medicines - same active ingredient, same strength, same way of taking them. The FDA requires them to deliver the same results in the body. That means if you take a generic version of metformin for diabetes or lisinopril for high blood pressure, your body treats it the same as the brand-name version. The key difference? Price. Generics typically cost 80-85% less. A brand-name statin might run $200 a month. The generic? $15. That’s not a small difference - it’s the line between taking your medicine every day and skipping doses because you can’t afford it. The system that made this possible started in 1984 with the Hatch-Waxman Act. Before that, drug companies could lock in high prices forever by holding patents. Hatch-Waxman changed that. It created a faster, cheaper path for generics to get approved. Instead of running full clinical trials (which cost billions), generic makers just had to prove their version worked the same way in the body. That’s called bioequivalence.How Generics Save Billions - And How We Know It Works
In 2024, generics saved the U.S. healthcare system $98 billion in direct spending. That’s not a guess. It’s from the Association for Accessible Medicines’ official report. Over the past decade, generics have saved over $400 billion annually. To put that in perspective: if you took all the money saved by generics in 2023 and gave it to every American as a cash payment, each person would get about $1,200. The numbers don’t lie. When a brand-name drug loses its patent, prices drop fast. Within a year, generics bring the cost down by 90%. Compare that to Medicare drug price negotiation, which the Congressional Budget Office says cuts prices by about 42% - still a big win, but nowhere near what generics do. And it’s not just about the price tag. When drugs are affordable, people take them. GoodRx found that 68% of patients skip or split pills when generics aren’t available. That leads to hospital visits, complications, and higher long-term costs. Generics don’t just save money - they save lives.The Hidden Challenges: Why Generics Don’t Always Reach Patients
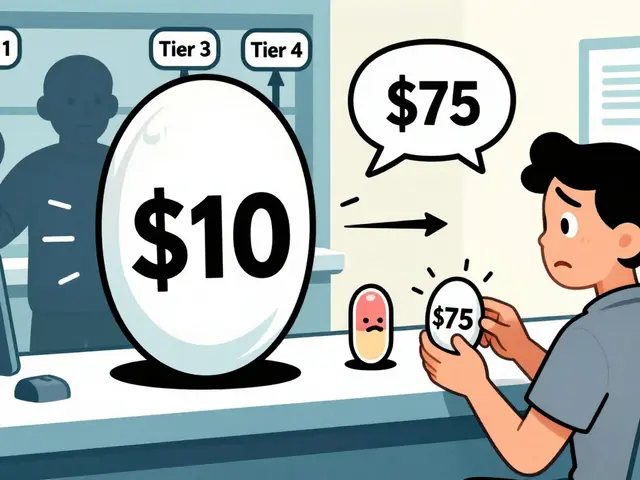
Even with all the savings, there are roadblocks. One big one? Patent tricks. Brand-name companies often file dozens of patents - sometimes over 140 - on minor changes to a drug’s coating, dosage, or delivery system. These aren’t real innovations. They’re legal tricks to delay generics. The Federal Trade Commission says these tactics push back generic entry by an average of 17 months. Then there’s the “pay-for-delay” problem. Sometimes, brand-name companies pay generic makers to stay off the market. It sounds crazy, but it happens. The FTC estimates this costs consumers $3.5 billion a year in lost savings. Another issue? Pharmacy benefit managers (PBMs). These middlemen negotiate drug prices for insurers. But instead of passing savings to patients, some plans charge higher copays for generics than for brand-name drugs - if the rebate the PBM gets from the brand is bigger than the actual price difference. Yes, you read that right. You pay more for the cheaper drug. And it’s not just about pills. Complex drugs like inhalers, injectables, and biologics are harder to copy. That’s where biosimilars come in. These are like generics for complex biologic drugs - think insulin, rheumatoid arthritis treatments, cancer drugs. They’re not identical, but they’re close enough to be safe and effective. And they cost 15-35% less than the brand. Here’s the problem: while 92% of small-molecule drugs face generic competition within a year of patent expiry, 90% of upcoming biologics have no biosimilar in development. That’s a huge gap. The FDA is trying to fix it, but progress is slow.
Real People, Real Savings
Behind every number is a person. On Reddit, one user shared how switching their mom from brand-name Humalog insulin ($350/month) to generic insulin lispro ($25/month) kept her from rationing doses. That’s not an outlier. A 2024 survey found 42% of Medicare Part D beneficiaries skipped doses because of cost - but only 12% did so with generics. Drugs.com reviews show generics get nearly the same efficacy ratings as brand-name drugs - 4.2 out of 5, versus 4.3. But when it comes to affordability? Generics score 4.5 out of 5. Brands? 2.3. That gap tells you everything. Still, there are complaints. Some people report stomach upset or other side effects after switching to a generic. That’s usually because of inactive ingredients - the fillers, dyes, or binders that don’t affect how the drug works but can irritate sensitive people. The FDA logged over 1,200 adverse events linked to generics in 2023, mostly from these additives. For most people, it’s fine. But for those with allergies or sensitivities, it matters.Why Generics Work Best for Chronic Conditions
Generics shine in long-term treatments. Think statins for cholesterol, metformin for diabetes, ACE inhibitors for blood pressure. These are drugs people take for years. A $200-a-month brand-name drug becomes a $20-a-month generic. That’s $2,160 saved per year. Multiply that by millions of patients, and you’ve got a system that stays affordable. But they’re not perfect for everything. Drugs with a narrow therapeutic index - where even tiny changes can cause harm - are trickier. Warfarin (a blood thinner) and levothyroxine (for thyroid issues) fall into this category. Some patients report symptoms returning after switching to a generic, even though the FDA says they’re equivalent. That’s why some states require doctors to specifically approve generic switches for these drugs.
Who Makes These Generics? And Where Do They Come From?
The biggest generic manufacturers are Teva, Viatris, and Sandoz. But a huge chunk of the active ingredients - up to 80% - come from just two countries: India and China. That’s fine when things run smoothly. But during the pandemic, supply chain snarls caused over 300 drug shortages, mostly affecting generics. The FDA is working on it. They’ve set up a Generic Drug Shortage Task Force and are pushing for more domestic production. But it’s expensive. Building a high-quality API factory in the U.S. costs hundreds of millions. Most generic makers still rely on overseas suppliers because it’s cheaper.What’s Next? The Future of Generics and Biosimilars
The Inflation Reduction Act capped insulin at $35 a month for Medicare patients - and that pushed private insurers to follow. Eli Lilly dropped its insulin price from $275 to $25. That’s not because of negotiation. It’s because generics and biosimilars were coming. The brand had to react. The FDA’s new Biosimilars Action Plan aims to cut approval times in half. That’s good news. But without policy changes to stop patent abuse and pay-for-delay deals, savings won’t reach their full potential. The Congressional Budget Office says if we fix the biosimilar void - the 90% of biologics with no competition in the pipeline - we could save an extra $234 billion over the next decade. That’s more than what Medicare negotiation alone will save.What You Can Do
If you’re on a prescription, ask your doctor or pharmacist: Is there a generic? If there is, insist on it unless there’s a medical reason not to. Ask your insurer: Do they charge higher copays for generics? If so, switch plans. Use tools like GoodRx or the FDA’s Orange Book to check therapeutic equivalence codes. Don’t assume brand-name means better. It usually means more expensive. And in healthcare, that’s the one thing we can’t afford.Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. They must also prove bioequivalence - meaning they work the same way in the body. Over 90% of generic drugs are rated "A" in the FDA’s Orange Book, meaning they’re therapeutically equivalent with no known substitution problems.
Why are generic drugs so much cheaper?
Brand-name drugs cost billions to develop and require years of clinical trials. Generics skip that. They only need to prove they work the same as the original, which takes months, not years, and costs a fraction. No marketing, no patent protection, no R&D overhead - so the savings get passed on.
Can I switch from a brand-name drug to a generic without my doctor’s permission?
In most cases, yes. Pharmacists can substitute a generic unless the prescription says "dispense as written" or the drug has a narrow therapeutic index (like warfarin or levothyroxine). In 12 states, prescriber approval is required for those high-risk drugs. Always check your state’s rules and talk to your pharmacist.
What’s the difference between a generic and a biosimilar?
Generics are exact copies of small-molecule drugs (like pills). Biosimilars are highly similar versions of complex biologic drugs (like injections for arthritis or cancer). They’re not identical because biologics are made from living cells - but they work the same way and are proven safe. Biosimilars cost 15-35% less, while generics cost 80-85% less.
Why don’t all insurance plans cover generics first?
Some plans don’t because pharmacy benefit managers (PBMs) make more money from brand-name drugs through rebates. Even if a generic costs less, the PBM might get a bigger rebate from the brand, so they charge you more for the generic. This is called a "generic differential." Always check your plan’s formulary and ask your insurer why.
Do generics cause more side effects?
The active ingredient causes the same effects. But generics can use different inactive ingredients - like fillers or dyes - which may cause mild reactions in sensitive people. The FDA logged over 1,200 reports of side effects linked to generics in 2023, mostly from these additives. If you notice new symptoms after switching, talk to your doctor. It’s rare, but it happens.
How long does it take for a generic to become available after a brand drug’s patent expires?
On average, it takes 28 months. That’s because brand companies often use legal tactics - like filing extra patents or suing generic makers - to delay entry. The FTC found these delays cost consumers billions each year. But once the first generic enters, prices drop fast - often by 90% within a year.


11 Comments
Generics are a textbook example of regulatory efficiency. The Hatch-Waxman Act created a bioequivalence pathway that bypassed redundant Phase III trials without compromising safety. The FDA’s Orange Book therapeutic equivalence codes (TE codes) are the gold standard-A-rated generics are pharmacologically identical. The real issue isn’t efficacy; it’s market distortion via evergreening patents and PBM rebate structures that invert cost incentives.
Man, I’ve seen this play out with my dad’s diabetes meds. He was skipping doses because the brand-name metformin was $180 a month. Switched to generic-$12. He’s been stable for two years now. It’s not just about money, it’s about dignity. People shouldn’t have to choose between food and their health. This system works when it’s allowed to.
Let’s be clear: the pharmaceutical industry’s lobbying apparatus is a machine designed to extract rent. Patent thickets, pay-for-delay, PBM kickbacks-it’s all engineered to suppress competition. The FTC has documented this for decades. The fact that we still tolerate it is a policy failure of epic proportions. Generics aren’t the problem. The rent-seekers are.
I grew up in rural Kentucky. My grandma took lisinopril for 15 years. When the generic hit, her copay dropped from $45 to $4. She started filling prescriptions on time. No more skipping doses. No more ER visits. That’s the real ROI of generics-not just dollars saved, but lives stabilized. We talk about healthcare reform like it’s abstract. It’s not. It’s your neighbor, your parent, your aunt.
Just ask your pharmacist if there’s a generic. If there is, take it. No drama. It’s the same medicine. Cheaper. Works the same. Done.
Bro, in India we make like 60% of the world’s generics. Our factories are FDA-approved, but in US they still act like they’re sketchy? Like, the active ingredient is same, man. Why you pay 10x? My cousin in Delhi takes same metformin as my uncle in Chicago-same pill, different price tag. Capitalism gone wild.
AMERICA IS THE ONLY COUNTRY THAT LETS PHARMA ROB PEOPLE LIKE THIS. 🇺🇸💔 We pay $200 for insulin while Canada pays $30. And we let them? We let them? This isn’t capitalism-it’s corporate feudalism. Time to burn it all down. #MedicareForAll #GenericsAreNotScams
Oh wow, so the solution to our $650B drug problem is… to buy the exact same pills for 85% less? Groundbreaking. I’m shocked this hasn’t been discovered before the invention of the wheel. Truly, the genius of the American healthcare system.
Let’s not pretend this is about patients. This is about power. The FDA, the FTC, the DOJ-all captured. The real tragedy isn’t that generics exist-it’s that they’re the exception, not the rule. We live in a system where the only thing more profitable than curing disease is keeping people chronically sick. The biosimilar void? It’s not an oversight. It’s intentional. They don’t want competition. They want dependence.
People say generics are fine, but have you read the inactive ingredients? Corn starch, talc, artificial dyes-some of these are banned in the EU. You think your body doesn’t notice the difference? It’s not the active ingredient that causes inflammation-it’s the junk they add to cut costs. You’re not saving money. You’re sacrificing your gut.
Generics? Lol. Did you know the FDA outsources inspections to China and India? Those labs are rigged. The pills you take? They’re made in factories that don’t even have running water. The whole system is a lie. Big Pharma + the government + the WHO-they’re all in cahoots. You think insulin is $35 now because of ‘competition’? Nah. They just want you to think you’re winning so you don’t ask why your bloodwork’s off.