Understanding Restless Leg Syndrome
Restless Leg Syndrome (RLS) is a neurological disorder characterized by an uncontrollable urge to move one's legs. This sensation usually occurs during periods of inactivity, such as when lying down in bed or sitting for extended periods of time. The symptoms of RLS can range from mild to severe, and the condition can significantly impact a person's sleep quality and overall well-being.
In this article, we will explore the impact of Restless Leg Syndrome on sleep quality and discuss various strategies for managing and alleviating the symptoms of this disorder.
How RLS Affects Sleep
People with Restless Leg Syndrome often find it difficult to fall asleep or stay asleep due to the constant need to move their legs. These involuntary movements can disrupt the natural sleep cycle, causing individuals to experience fragmented and unrefreshing sleep. As a result, people with RLS may suffer from chronic sleep deprivation, which can lead to a host of physical, mental, and emotional health issues.
Furthermore, the symptoms of RLS tend to worsen during the night, making it even more challenging for individuals to achieve restful sleep. This can result in significant daytime fatigue, making it difficult to function effectively during the day.
The Connection Between RLS and Insomnia
Insomnia is a common sleep disorder that affects millions of people worldwide. It is characterized by the inability to fall asleep or stay asleep, leading to poor sleep quality and chronic sleep deprivation. There is a strong connection between Restless Leg Syndrome and insomnia, as the symptoms of RLS can make it difficult for individuals to achieve restful sleep.
Moreover, the anxiety and stress associated with RLS can exacerbate insomnia, creating a vicious cycle that can be difficult to break. As a result, treating both RLS and insomnia is essential for improving sleep quality and overall well-being.
Managing RLS with Lifestyle Changes
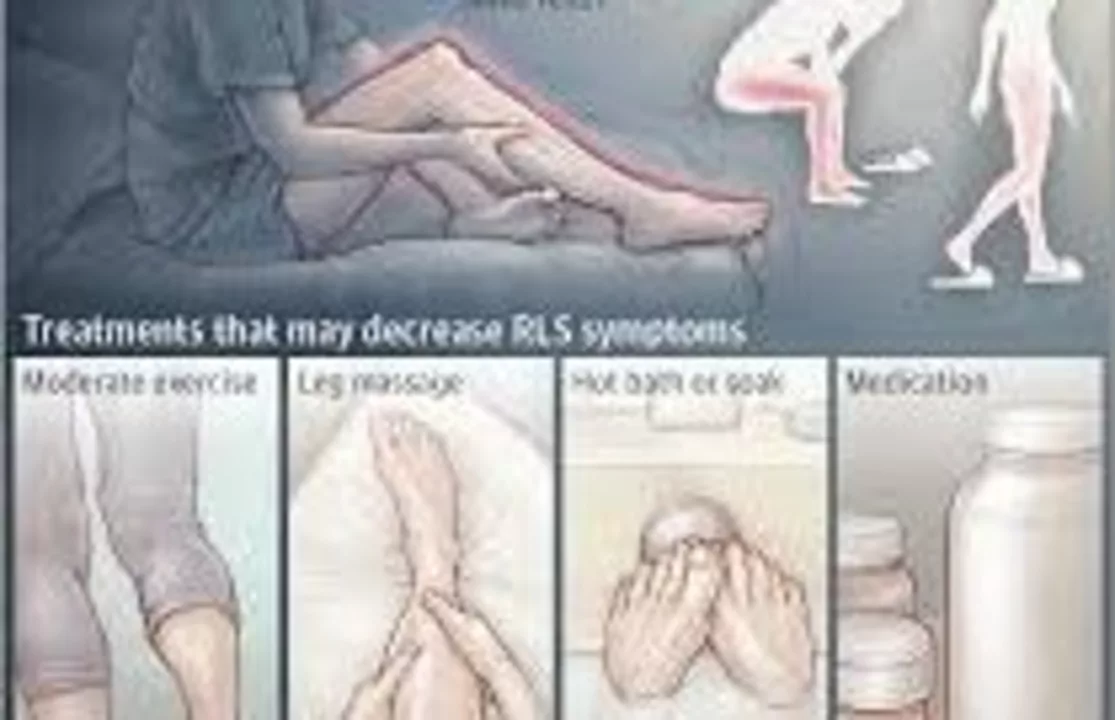
Although there is no cure for Restless Leg Syndrome, there are several lifestyle changes that can help alleviate the symptoms and improve sleep quality. Some of these changes include maintaining a regular sleep schedule, creating a relaxing bedtime routine, and avoiding caffeine, alcohol, and nicotine close to bedtime. Additionally, engaging in regular physical activity can help reduce RLS symptoms by promoting muscle relaxation and improving overall circulation.
It is also important for individuals with RLS to create a comfortable and supportive sleep environment, as this can help reduce the severity of symptoms and promote better sleep quality.
Medications for RLS and Sleep Improvement
In some cases, medications may be necessary to manage the symptoms of Restless Leg Syndrome and improve sleep quality. These medications can include dopamine agonists, such as ropinirole and pramipexole, which help regulate the levels of dopamine in the brain. Other medications that may be prescribed for RLS include benzodiazepines, opioids, and anticonvulsants.
It is important to note that not all individuals with RLS will require medication, and the effectiveness of these treatments can vary from person to person. Therefore, it is crucial to consult with a healthcare professional before starting any new medication regimen.
Coping Strategies for RLS-Induced Sleep Problems
Living with Restless Leg Syndrome can be challenging, but there are several coping strategies that can help manage the condition and improve sleep quality. One such strategy is practicing relaxation techniques, such as deep breathing exercises, progressive muscle relaxation, and meditation. These techniques can help calm the mind and body, making it easier to fall asleep and stay asleep.
Another coping strategy is to keep a sleep diary, which can help individuals track their sleep habits and identify any patterns or triggers that may be contributing to their RLS symptoms. By identifying and addressing these triggers, individuals can work towards improving their sleep quality and overall well-being.
Seeking Professional Help for RLS and Sleep Issues
If you are struggling with Restless Leg Syndrome and experiencing significant sleep disruptions, it is important to seek professional help from a healthcare provider or sleep specialist. These professionals can help determine the underlying cause of your RLS symptoms and recommend appropriate treatment options to improve your sleep quality and overall health.
Remember, you don't have to suffer in silence – reaching out for help can be the first step towards better sleep and a happier, healthier life.






17 Comments
Restless Leg Syndrome, often abbreviated as RLS, presents itself as a compelling illustration of how peripheral neural pathways can exert profound influence over central sleep mechanisms. The involuntary urge to move the lower extremities during periods of repose reflects a dysregulation within dopaminergic circuits that extends beyond mere discomfort. Consequently, individuals afflicted with this condition frequently encounter fragmented sleep architecture, a phenomenon that undermines the restorative phases essential for physiological homeostasis. Chronic sleep interruption, in turn, precipitates a cascade of neurocognitive deficits, ranging from attenuated attention spans to impaired memory consolidation. Moreover, the persistent nocturnal restlessness contributes to heightened sympathetic arousal, thereby fostering a milieu conducive to hypertension and cardiovascular strain. From a psychosocial perspective, the unpredictable nature of RLS episodes can engender a sense of helplessness, often exacerbating comorbid mood disorders such as anxiety and depression. Therapeutic interventions, therefore, must embrace a multimodal paradigm that integrates pharmacological agents, behavioral modifications, and environmental optimizations. Pharmacotherapy, particularly the utilization of dopamine agonists, aims to rectify the underlying neurotransmitter imbalance, yet clinicians must remain vigilant regarding potential side effects, including augmentation phenomena. Concurrently, lifestyle adjustments-such as the institution of consistent sleep schedules, reduction of caffeine intake, and engagement in moderate exercise-serve to attenuate symptom severity. The creation of a supportive sleep environment, characterized by ergonomic bedding and ambient temperature control, further mitigates nocturnal disturbances. It is also incumbent upon healthcare providers to educate patients about sleep hygiene practices, including the avoidance of electronic device exposure prior to bedtime. In addition, the implementation of relaxation techniques, such as progressive muscle relaxation and guided imagery, can facilitate the transition into sleep. Ultimately, a comprehensive, patient-centered approach that acknowledges the intricate interplay between neurophysiology, behavior, and environment stands as the most efficacious strategy for ameliorating the impact of RLS on sleep quality.
Man, RLS is like that annoying buddy who just won\'t quit you, especially when you finally try to catch some Z's. I swear, the legs start doing the jitterbug just when you’re about to drift off. It feels like a relentless urge to dance, but in the dark, nobody’s cheering you on. Definitely makes the night feel endless, and mornings turn into a coffee‑fueled marathon. The whole thing messes with your mood, too – you’re cranky before the sun even rises.
From a functional standpoint, the pathophysiology of Restless Leg Syndrome implicates iron‑deficiency mediated dopaminergic dysfunction, which can be quantified via serum ferritin thresholds. Clinicians often employ augmentation protocols that integrate gabapentin enacarbil alongside behavioral sleep‑restriction therapy to maximize REM efficiency. Moreover, the utilization of actigraphy provides objective metrics on periodic limb movements, facilitating evidence‑based titration of dopamine agonists. In practice, multidisciplinary collaboration-neurology, sleep medicine, and physical therapy-yields superior outcomes compared to monotherapy. It’s crucial to monitor for augmentation, characterized by earlier symptom onset and increased severity, particularly in long‑term ropinirole use. Patient education regarding nighttime stretching regimens and temperature regulation can also modulate peripheral nerve excitability, thereby reducing symptomatic frequency.
Indeed, Liam-your points underscore the necessity of a holistic regimen!; consider the synergistic effects of low‑dose melatonin combined with a structured leg‑muscle‑relaxation routine; this pairing often curtails nocturnal jerks, fostering deeper sleep cycles. Additionally, the strategic timing of caffeine abstinence-ideally 6‑hours pre‑bedtime-mitigates central nervous system stimulation. Let’s not overlook the value of compression stockings; they enhance venous return, which may alleviate peripheral discomfort. Together, these measures construct a robust defense against the relentless leg‑twitch tyranny.
While the conventional wisdom extols lifestyle tweaks and dopamine agonists, one must question whether we are simply applying band‑aid solutions to a deeper neurophysiological conundrum. The literature often glosses over the potential iatrogenic risk of long‑term dopaminergic therapy, such as impulse control disorders, which can be as debilitating as the original syndrome. Moreover, the romanticization of “relaxation techniques” veers into the realm of pseudo‑science when not anchored in randomized trials. It is imperative to maintain a critical eye, lest we perpetuate a cycle of temporary fixes while neglecting emergent biomarkers that could herald a paradigm shift in RLS management.
That’s a thoughtful reminder, Dominique. Even if the current options seem limited, sharing reliable resources and encouraging patients to track their symptoms can empower them to work closely with their clinicians. Small steps, like consistent sleep hygiene and gentle stretching, often build momentum toward better nights.
RLS really does feel like a relentless storm that never quite lets you rest. The way the legs twitch and tangle in the dark is nothing short of dramatic, turning a simple night into a battlefield of discomfort. Even the most diligent sleep schedule can be undone by that insistent urge to move. It’s a struggle that clouds both body and mind, leaving you exhausted and irritable by sunrise.
Got it.
Restless leg syndrome is a classic example of how peripheral nerve hyperexcitability can sabotage the sleep‑recovery cycle. 🦵💤 The best approach often starts with a thorough assessment of iron levels, because ferritin deficiency is a frequent culprit. From there, a judicious trial of low‑dose dopamine agonists can be considered, with careful monitoring for augmentation. Complementary strategies-such as evening leg‑stretch routines, cool bedroom temperatures, and mindfulness‑based relaxation-have robust evidence supporting their efficacy. It’s also wise to keep a detailed sleep diary; patterns emerge that can guide therapeutic adjustments. 😉
absolutely, abhi, the diary thing is gold, you can see triggers fast and tweak habits on the fly. also, trying a warm bath before bed can chill the nerves a bit, but keep the water temp low enough not to wake you up. keep caffeine out after 3pm, and maybe try a short walk after dinner. these little hacks add up.
The interplay between restless leg syndrome and sleep fragmentation is multifaceted, encompassing neurochemical, vascular, and behavioral dimensions. Empirical studies have demonstrated that iron deficiency, reflected by suboptimal serum ferritin concentrations, correlates with heightened limb movement index scores, underscoring the necessity of routine hematologic evaluation. Moreover, circadian misalignment-stemming from irregular sleep–wake schedules-exacerbates dopaminergic dysregulation, thereby intensifying nocturnal leg sensations. Interventions that prioritize chronological consistency, such as fixed bedtime and wake‑time parameters, have been shown to attenuate symptom severity. In addition, the incorporation of low‑impact aerobic exercises in the early evening can augment peripheral circulation, potentially mitigating the hyper‑excitability of motor neurons. It is incumbent upon clinicians to adopt a personalized, evidence‑based regimen that synergizes pharmacologic agents, like gabapentin enacarbil, with non‑pharmacologic modalities, including progressive muscle relaxation and temperature modulation. Ultimately, a comprehensive therapeutic algorithm that integrates biochemical assessment, lifestyle optimization, and patient education offers the most robust avenue for improving sleep quality in individuals afflicted with RLS.
Oh great, another sleepless night thanks to restless legs-just what the doctor ordered. As if the day‑to‑day grind wasn’t enough, now your limbs decide it’s audition time for a tap‑dance troupe. Sure, “relaxation techniques” might help, but who’s got the time when you’re already running on fumes?
Honestly, the whole discourse around RLS feels like a rehash of the same old clichés. People keep throwing around terms like "dopamine" and "sleep hygiene" as if they're groundbreaking revelations. It's high time we question whether these buzzwords actually translate into meaningful outcomes for patients, or if they're merely comforting platitudes.
While the discussion is interesting, it overlooks the simple fact that many patients just need clear, actionable advice. Complex jargon won't help someone who's lying awake, legs twitching, and looking for a quick fix.
Look, all this talk about iron levels and dopamine agonists is just textbook fluff. In reality, most people will never see a specialist, they’ll just keep suffering because the system is too lazy to give them real solutions.
Hey there, I get how frustrating it can be when the usual tips don’t cut it. Have you tried keeping a consistent bedtime routine and maybe some gentle calf stretches before hitting the sheets? Sometimes the simplest changes can make a big difference.
In reviewing the evidence, it becomes apparent that a multimodal approach-encompassing pharmacologic intervention, lifestyle modification, and patient education-is essential for optimal management of Restless Leg Syndrome. 🩺📚 Careful monitoring for side‑effects, particularly augmentation, remains paramount. Moreover, integrating objective sleep assessments, such as polysomnography or actigraphy, can refine treatment pathways and ensure that therapeutic adjustments are data‑driven. Ultimately, a collaborative, patient‑centered model stands as the gold standard for addressing the complex interplay between RLS and sleep quality.