Cumulative Drug Toxicity Calculator
How It Works
This tool calculates how a drug accumulates in your body based on its half-life and dosing schedule. Understanding this helps identify when your medication might reach dangerous levels.
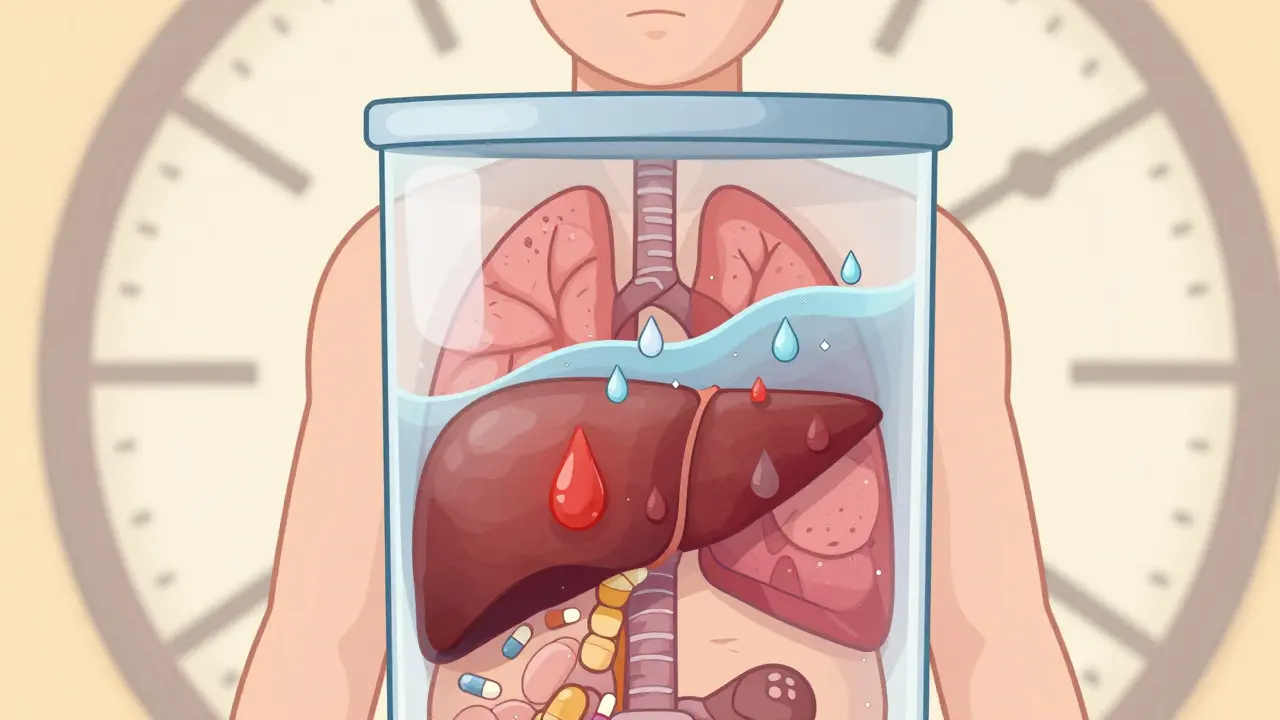
Most people assume that if a medication is safe for a few weeks, it’s safe for years. But that’s not always true. Some drugs don’t hurt you right away-they slowly build up in your body like water filling a bucket, drop by drop, until it overflows. This is cumulative drug toxicity, and it’s one of the quietest, most dangerous side effects in modern medicine.
What Is Cumulative Drug Toxicity?
Cumulative drug toxicity happens when your body can’t get rid of a medicine fast enough. Instead of clearing out after each dose, the drug lingers. Over days, weeks, or even years, it piles up. Eventually, the level in your blood or tissues crosses a line-from therapeutic to toxic. This isn’t like a sudden allergic reaction or a bad stomachache after your first pill. Those are acute effects. Cumulative toxicity is silent. You might take the same dose for months without noticing anything. Then, out of nowhere, you feel exhausted, your skin turns yellow, your heart skips, or your lungs start to scar. By then, the damage is already done. Drugs that are fat-soluble are especially risky. Think vitamin A, digoxin, amiodarone, or even some chemotherapy agents. These don’t dissolve in water, so your kidneys can’t flush them out easily. Instead, they hide in your fat tissue or liver, slowly leaking back into your bloodstream. Some can stay in your body for months-even years-after you stop taking them.Why Does This Happen?
It all comes down to pharmacokinetics: how your body absorbs, moves, breaks down, and gets rid of a drug. The key player here is the half-life-the time it takes for half the drug to leave your system. If a drug’s half-life is over 24 hours, it’s already at risk for building up. Some, like amiodarone, have half-lives of 50 to 100 days. That means if you take it daily, after two months, you’re carrying nearly four times the amount you took on day one. Your liver and kidneys do the heavy lifting in clearing drugs. But if they’re not working at 100%, things get dangerous fast. In older adults or people with chronic kidney disease, liver cirrhosis, or even long-term alcohol use, drug clearance can drop by 30% to 50%. That’s not a small difference-it’s the difference between a safe dose and a toxic one. And it’s not just about the medicine itself. Environmental toxins, poor diet, and even some herbal supplements can overload your detox systems. Ayurvedic medicine calls this Dushi Visha-chronic, low-grade poison that builds over time. Modern science is catching up. The same pathways that clear drugs also handle heavy metals, pesticides, and industrial chemicals. When those systems are already taxed, even normal doses of medication can become dangerous.Who’s Most at Risk?
You might think this only affects cancer patients on chemo. It doesn’t. It affects anyone on long-term medication. - Elderly patients: 68% of adverse drug reactions in people over 65 are due to cumulative effects, according to the Journal of the National Cancer Institute. Many are on five or more drugs at once. Each one adds to the pile. - People with chronic conditions: Those with heart failure, rheumatoid arthritis, or atrial fibrillation often take drugs like digoxin, methotrexate, or amiodarone for years. These are high-risk for toxicity. - Patients on multiple prescriptions: Drug interactions can slow down metabolism. A common painkiller like ibuprofen can interfere with how your liver processes blood thinners. Suddenly, your warfarin level spikes-even though you didn’t change the dose. - People with genetic differences: Some people have slower versions of liver enzymes (like CYP2D6 or CYP3A4) that break down drugs. They’re essentially born with a higher risk of accumulation. Most doctors never test for this.
Real Cases, Real Consequences
A 72-year-old woman in Perth was on amiodarone for atrial fibrillation for seven years. Her doctor checked her thyroid and liver every six months. Everything looked fine. Then she started coughing nonstop. A CT scan showed her lungs were scarred-pulmonary fibrosis. The cause? Cumulative amiodarone toxicity. She’d taken over 600 grams total. That’s the known danger threshold. Her blood levels were normal at every check-up, but the drug had been sitting in her lung tissue all along. Another case: a 58-year-old man on methotrexate for psoriatic arthritis. He took it weekly, as prescribed. No side effects for five years. Then, one morning, he couldn’t get out of bed. His blood work showed his white blood cell count had crashed. His liver enzymes were through the roof. He’d accumulated enough methotrexate to suppress his bone marrow. He spent six weeks in the hospital. These aren’t rare. The FDA’s adverse event database recorded over 12,000 cases of cumulative toxicity between 2018 and 2022. Nearly half involved blood thinners, heart meds, or cancer drugs.How Doctors Miss It
Most doctors rely on blood tests to check if a drug is at a “safe” level. But here’s the problem: those tests measure what’s in your blood right now. They don’t show what’s hiding in your fat, liver, or lungs. That’s why a patient can have “normal” levels for years and still develop toxicity. The drug isn’t floating in the bloodstream-it’s stored. It’s like checking the water level in a bathtub while ignoring the sponge soaking up water under the floor. Also, many patients don’t tell their doctors about every pill they take. Herbal teas, over-the-counter painkillers, supplements-these all interact. One nurse on a Reddit forum shared that patients often say, “I’ve been taking this for 10 years and never had a problem.” But that’s exactly when the problem starts.
What Can Be Done?
The good news? This isn’t inevitable. There are ways to stop it before it starts. 1. Know your drug’s half-life. If it’s longer than 24 hours, ask your doctor or pharmacist about cumulative risk. For drugs like digoxin or lithium, regular blood tests are standard. For others, like amiodarone, you need more than blood tests-you need lung scans, eye exams, and liver ultrasounds over time. 2. Track your total lifetime dose. Some drugs have hard limits. For example, the lifetime cumulative dose of doxorubicin (a chemo drug) should never exceed 450 mg/m². Beyond that, heart damage becomes likely. Many oncology clinics now use digital trackers that automatically log each dose and warn when you’re nearing the limit. 3. Ask about alternatives. Is there a newer drug with less accumulation risk? For example, newer anticoagulants like apixaban or rivaroxaban don’t build up the way warfarin does. They’re safer for long-term use. 4. Use a pharmacist. Pharmacists are the unsung heroes of cumulative toxicity prevention. A 2023 study found that when pharmacists actively tracked cumulative doses in rheumatology and cardiology clinics, hospital admissions for drug toxicity dropped by 29%. 5. Get your liver and kidneys checked yearly. If you’re on long-term meds, annual blood tests for creatinine, ALT, AST, and eGFR aren’t optional. They’re essential.The Bigger Picture
The global market for therapeutic drug monitoring is expected to hit $4.7 billion by 2028. Why? Because hospitals and clinics are waking up. The European Medicines Agency now requires cumulative toxicity assessments for all new drugs meant for long-term use. The FDA is pushing pharmaceutical companies to include cumulative dose warnings on labels-up from 52% in 2017 to 78% in 2022. But technology isn’t keeping up. Only 38% of electronic health records in the U.S. can automatically calculate your total drug exposure. Most still rely on paper charts or scattered pharmacy records. That’s a gap. And it’s dangerous. Meanwhile, AI is starting to help. Researchers at Memorial Sloan Kettering are testing models that predict your personal risk of toxicity based on 27 different factors-your genes, your age, your kidney function, your diet, even your sleep patterns. Early results show 82% accuracy. That’s not science fiction. It’s the future.What You Should Do Now
If you’re on any medication for more than six months, here’s what to do:- Ask your doctor: “Is this drug known to build up in the body?”
- Ask: “What’s my total lifetime dose so far?”
- Ask: “Are there any tests I should be getting beyond blood work?”
- Keep a personal log: Write down every pill you take, the dose, and when you started.
- Don’t assume “no side effects” means “safe.”
Can cumulative drug toxicity be reversed?
Sometimes, yes-but not always. If caught early, stopping the drug and supporting your liver and kidneys can allow your body to slowly clear the buildup. For example, stopping amiodarone can lead to gradual improvement in lung function over months. But if the damage is severe-like scarring in the lungs or heart muscle-it’s often permanent. Early detection is everything.
Are over-the-counter drugs capable of cumulative toxicity?
Absolutely. Acetaminophen (Tylenol) is the most common example. Taking just 1,000 mg daily for months can cause silent liver damage, especially if you drink alcohol or have a fatty liver. NSAIDs like ibuprofen can cause kidney damage over time with daily use. Even herbal supplements like kava or comfrey can build up and harm your liver. Just because something is sold without a prescription doesn’t mean it’s safe long-term.
Why don’t doctors test for cumulative toxicity more often?
Most doctors aren’t trained to think about cumulative effects. Medical education focuses on acute reactions and immediate side effects. Also, routine blood tests don’t detect stored drug levels. Specialized tests like tissue biopsies or advanced imaging aren’t standard practice. And without automated systems in electronic health records, tracking cumulative doses is time-consuming and easy to miss.
How long does it take for cumulative toxicity to develop?
It varies. For some drugs, like digoxin, toxicity can appear in weeks if kidney function is poor. For others, like amiodarone or chemotherapy agents, it may take 6 months to 5 years. The timeline depends on the drug’s half-life, your metabolism, your age, and whether you have other health conditions. There’s no universal clock-it’s personal.
Can I avoid cumulative toxicity by taking breaks from my medication?
Sometimes, but not always. For drugs with very long half-lives-like amiodarone-taking a break won’t help much because the drug is still sitting in your fat tissue for months. For others, like certain antibiotics or antivirals, a drug holiday might help reset your system. Never stop or change your meds without talking to your doctor. The risks of stopping can be worse than the risk of accumulation.
Is cumulative toxicity more common in older adults?
Yes, and for several reasons. Older adults often have reduced kidney and liver function. They’re more likely to be on multiple medications. Their body fat percentage increases, and fat-soluble drugs accumulate more easily. Studies show 68% of adverse drug reactions in people over 65 are due to cumulative effects. That’s why the American Geriatrics Society Beers Criteria lists 34 medications as high-risk for seniors.






13 Comments
This is why America needs to stop letting big pharma run the show. They don't care if you live or die as long as you keep buying pills.
One dose. One problem. That's it.
Of course it's toxic. Everyone knows you can't trust doctors anymore. They're just pushing pills to hit their quotas. My aunt took that amiodarone stuff for three years and ended up in a coma. No one warned her. Just another American healthcare failure.
I really appreciate how thorough this is. I'm on methotrexate for psoriasis and had no idea about cumulative toxicity. I'm going to ask my rheumatologist about liver scans and total dose tracking. Thank you for sharing this - it could save lives.
This is spot on. I'm a pharmacist and I see this every day. Patients come in with 8 prescriptions, no idea what any of them do, and think 'no side effects' means 'safe.' The real danger is the silent buildup. We need more pharmacist-led med reviews. It's not glamorous, but it prevents ER visits. Seriously, if you're on long-term meds, talk to your pharmacist. They're the ones who actually track this stuff.
Half life matters but most docs dont even know what it is. I took digoxin for 4 years and my doc never checked levels. Just said 'you feel ok right?' Yeah i feel fine until i start vomiting and my heart skips. Now i know better. Get your own data.
You know what's really toxic? The belief that medicine is neutral. This whole post reads like a corporate pamphlet disguised as science. Drugs are tools of control. The body doesn't 'accumulate' - it resists. And the system punishes resistance with more pills. You think your liver is just a filter? It's a battlefield. And they're winning because you're too distracted to notice you're bleeding out slowly.
This is so important 😔 I'm 32 and on a daily med for anxiety - never thought about long-term buildup. Just started logging every pill I take in a notes app. Small step but feels like reclaiming control. Also - yes to pharmacists! They're the real MVPs. 🙏
They call it 'cumulative toxicity' like it's some scientific mystery. It's just poison. Slow, silent, and sanctioned. Your body isn't broken - it's being murdered by bureaucracy wrapped in white coats. That woman with the scarred lungs? They knew. They just didn't care enough to look past the blood test numbers. Welcome to modern medicine - where death is a side effect you have to sign a waiver for.
This is all a lie. The FDA and WHO are in cahoots with Big Pharma to make people dependent. They don't want you healthy. They want you on meds forever. The 'half-life' is a distraction. The real truth? They inject nanoparticles into the drugs to make them linger. Look up chemtrails. Same thing. They're building a slave population. Your liver is just the first target.
I've been on 7 meds for 11 years. Every doctor says 'you're fine.' I'm not fine. I'm tired all the time, my hands shake, and I forget my own birthday last month. But hey - my bloodwork is 'normal.' So I guess I'm just weak. Maybe I should just stop complaining and take more pills. That's what the system wants, right?
People like you think you're so smart because you read a medical article. But you're just another sheep. You don't understand the real problem. The problem is that you let them poison you. You didn't fight. You didn't question. You just swallowed it. You're not a victim. You're complicit.
I'm from India and we've known about this for centuries. Ayurveda calls it Dushi Visha - chronic poison from overuse. We didn't need fancy scans or half-life charts to know that if you keep pouring poison into your body, eventually it'll rot you from the inside. Modern medicine just gave it a fancy name and a price tag. The real solution? Less pills. More food. More movement. More sleep. And less trust in a system that profits from your sickness.
You're all missing the point. This isn't about drugs. It's about personal responsibility. If you're stupid enough to take meds for years without checking your liver enzymes, you deserve what you get. Stop blaming doctors. Stop blaming pharma. Blame yourself for being lazy, ignorant, and too lazy to read the damn label. Your body isn't a magic box. It's a machine. And you didn't even read the manual.