Thiopurine Metabolism: How Your Body Processes Key Immune Drugs
When you take a drug like azathioprine, an immunosuppressant used for autoimmune diseases and organ transplants. Also known as 6-MP, it doesn’t work directly—your body must break it down first. This process is called thiopurine metabolism, the biochemical pathway that converts thiopurine drugs into active or inactive forms. If this system is too fast or too slow, the drug can fail or cause serious harm.
At the heart of thiopurine metabolism is the TPMT enzyme, a liver enzyme that breaks down thiopurines to prevent toxic buildup. About 1 in 300 people have a genetic variation that makes TPMT nearly inactive. For them, standard doses of azathioprine or 6-MP, a direct form of the same drug used in leukemia treatment can cause life-threatening drops in white blood cells. Others have extra-active TPMT and clear the drug too quickly, meaning the treatment doesn’t work. That’s why doctors now test TPMT levels before starting these drugs—not as a suggestion, but as standard practice.
Thiopurine metabolism doesn’t happen in isolation. It’s affected by other medications, like allopurinol (used for gout), which can block the breakdown pathway and force toxic levels to rise. It’s also influenced by liver health, age, and even diet. These drugs are often prescribed for long-term conditions like Crohn’s disease or rheumatoid arthritis, so understanding how your body handles them isn’t just academic—it’s the difference between staying well and ending up in the hospital. The posts below show real cases where metabolism issues changed treatment outcomes, how labs detect enzyme activity, and what to do when standard doses don’t fit your biology. You’ll find practical advice on monitoring, alternatives, and how to talk to your doctor about your unique metabolic profile.
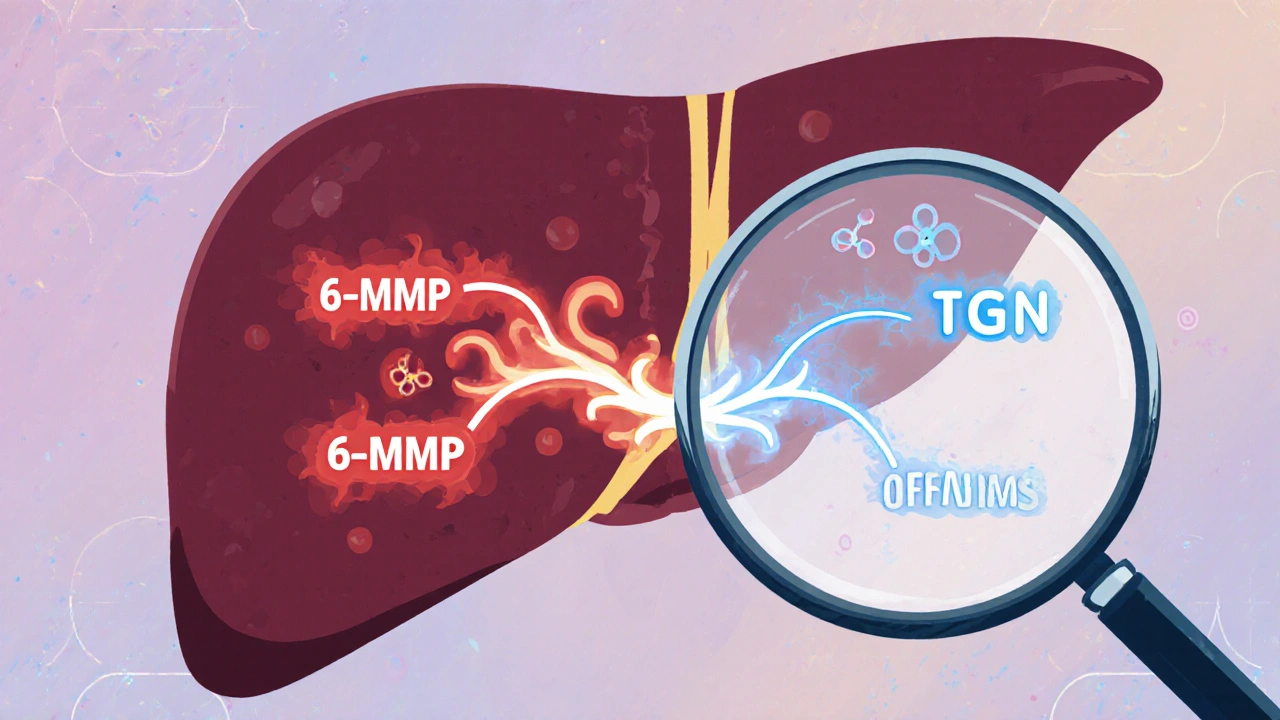
Azathioprine and Allopurinol: How Low-Dose Combination Therapy Prevents Toxic Metabolite Buildup
LDAA therapy combines low-dose azathioprine with allopurinol to redirect toxic metabolite production, improving efficacy and reducing liver damage in IBD and autoimmune hepatitis patients with high TPMT activity.