LDAA Therapy: What It Is, How It Works, and What You Need to Know
When we talk about LDAA therapy, Low-Dose, Long-Term Antimicrobial or Antidepressant therapy. Also known as low-dose prolonged treatment, it's not about quick fixes—it's about steady, careful management of chronic conditions using smaller amounts of medication over months or years. This approach is used in conditions where high doses cause too many side effects, but stopping treatment leads to relapse. Think of it like watering a plant daily instead of dumping a bucket on it once a week—you’re feeding the system without overwhelming it.
LDAA therapy isn’t just about the drug. It’s deeply tied to medication adherence, how consistently a patient takes their prescribed medicine. Without it, even the best low-dose plan fails. That’s why posts here cover real-world stories of people sticking to regimens for depression, chronic infections, or autoimmune issues—not because they were ordered to, but because they understood why it mattered. It’s also connected to drug interactions, how one medication affects another in the body. For example, if you’re on LDAA therapy and start taking an H2 blocker like famotidine, your body might not absorb the drug properly. Or if you smoke while on clozapine, your dose could become ineffective. These aren’t hypotheticals—they’re daily realities for people managing long-term care.
What makes LDAA therapy different from standard treatment? It’s the balance. Lower doses mean fewer side effects, but only if you take it every day. That’s why patient compliance, the extent to which a patient follows medical advice becomes the real measure of success. One post talks about how chloroquine phosphate works only if taken without gaps. Another explains why forgetting a single dose of atenolol can throw off your electrolytes. These aren’t isolated cases—they’re patterns. And they’re why LDAA therapy requires more than a prescription—it needs understanding, routine, and support.
You won’t find magic bullets here. What you will find are clear, practical guides on how to make LDAA therapy work in real life: how to track doses, spot dangerous interactions, adjust for lifestyle changes like smoking, and know when to ask for help. Whether you’re managing a mental health condition, a lingering infection, or a chronic illness, the tools and insights below are built for people who need to stay on track—not just for weeks, but for years.
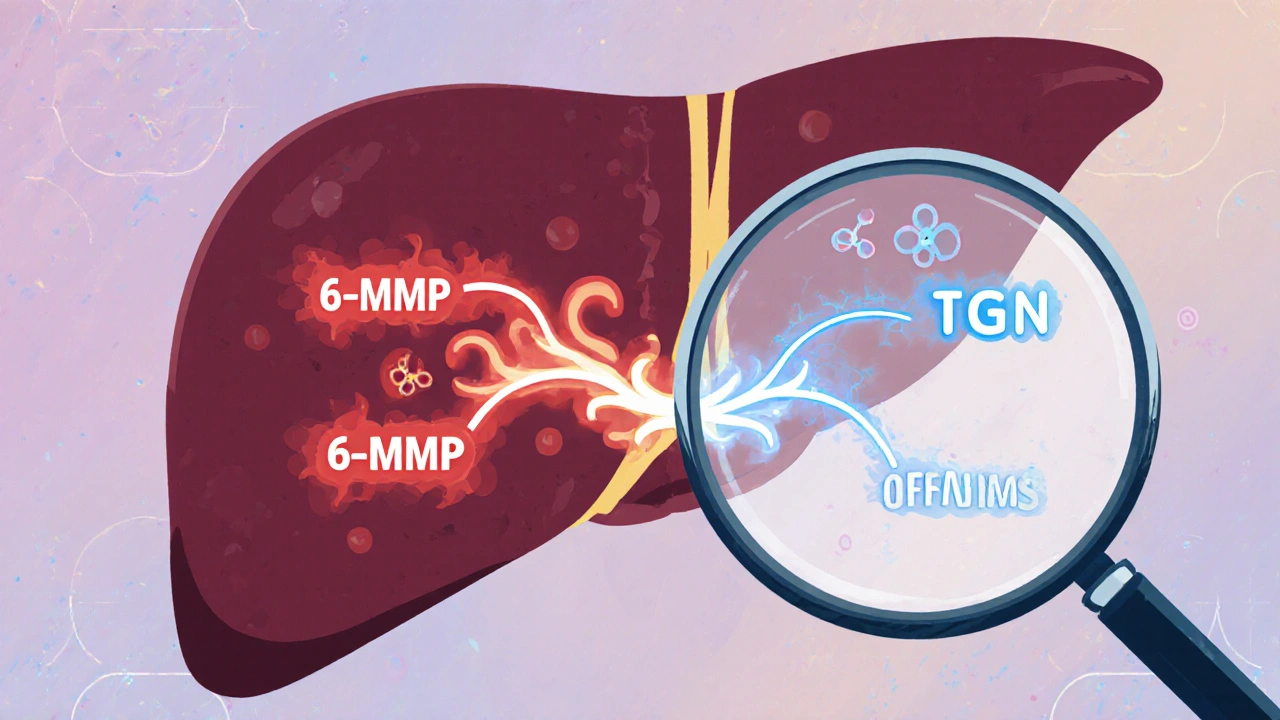
Azathioprine and Allopurinol: How Low-Dose Combination Therapy Prevents Toxic Metabolite Buildup
LDAA therapy combines low-dose azathioprine with allopurinol to redirect toxic metabolite production, improving efficacy and reducing liver damage in IBD and autoimmune hepatitis patients with high TPMT activity.