Brain Health and the Latest Insights
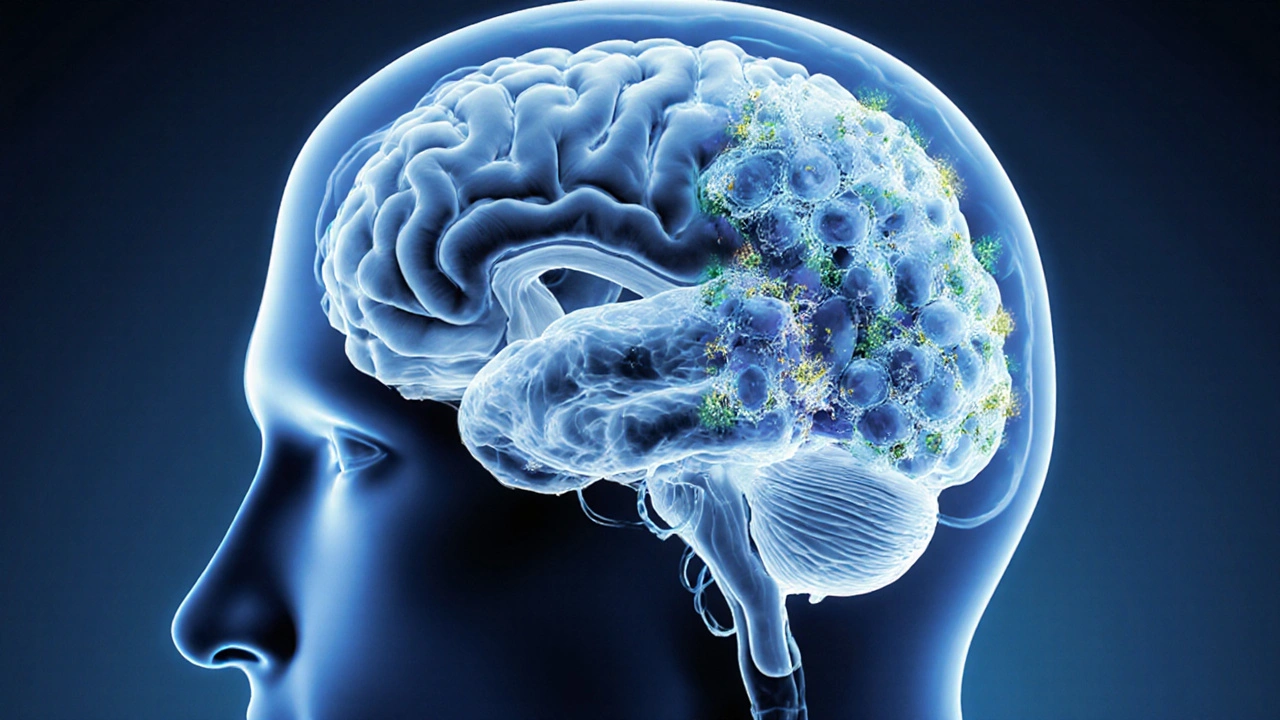
When talking about brain, the central organ that controls thoughts, feelings, and body functions. Also known as cerebrum, it processes information, stores memories, and regulates hormones. Connected to sleep, a restorative state that clears metabolic waste and strengthens neural connections, the brain depends on quality rest to maintain sharp cognition and emotional balance. Likewise, medication, any pharmaceutical that alters brain chemistry to treat conditions can boost or impair performance, depending on dosage and individual response. Finally, neurotransmitters, chemical messengers like dopamine, serotonin, and acetylcholine act as the brain's wiring, shaping alertness, mood, and memory. The brain encompasses cognition, motor control, and autonomic regulation; it requires proper sleep, balanced neurotransmitters, and thoughtful medication use to function at its best. These relationships set the stage for the articles you’ll find below.
How Sleep, Wake‑Promoting Drugs, and Neurochemistry Interact
Recent studies show that inadequate sleep spikes the brain’s adenosine levels, creating that groggy feeling many of us know. Wake‑promoting agents like armodafinil or modafinil work by blocking adenosine receptors and increasing dopamine transmission, essentially tricking the brain into a more alert state. This interplay illustrates the semantic triple: Sleep influences neurotransmitter balance, which in turn affects brain alertness. On the flip side, over‑reliance on stimulants can disturb natural sleep architecture, leading to impaired memory consolidation and mood swings. Understanding this feedback loop helps you weigh the benefits of a sleep tracker that translates nightly patterns into actionable data against the short‑term boost of a prescription wake‑fulness pill. Whether you’re managing daytime sleepiness or looking to fine‑tune cognitive performance, recognizing how sleep, medication, and neurotransmitters connect is crucial for sustainable brain health.
Beyond sleep and stimulants, many everyday medications—antidepressants, antipsychotics, and even insulin—reach the brain and modulate its chemistry. For instance, selective serotonin reuptake inhibitors (SSRIs) raise serotonin levels, easing depression but sometimes causing mild cognitive fog. Antipsychotics like olanzapine block dopamine receptors to reduce psychosis, yet they may affect metabolic pathways that indirectly impact brain energy supply. Insulin, while primarily a blood‑sugar regulator, also crosses the blood‑brain barrier and supports neuronal glucose uptake, influencing learning and memory. These examples fulfill another semantic triple: Medication alters neurotransmitter activity, which shapes brain function and overall cognition. By seeing the bigger picture—how each drug class interacts with the brain’s signaling network—you can make more informed choices, whether you’re selecting a generic antidepressant, evaluating a new diabetes regimen, or simply curious about the science behind everyday health decisions. The collection below dives deeper into each of these topics, offering practical tips, safety guidelines, and comparative reviews to help you keep your brain operating at its peak.
How Hyponatremia Affects Brain Function and Memory
Explore how low blood sodium impairs memory, attention, and brain health, the symptoms to watch for, and effective ways to treat hyponatremia before cognitive damage becomes permanent.