
When you pick up a prescription, you might see two options: the name you recognize from TV ads, or a plain bottle with a long chemical name. The brand-name drug costs $200. The generic? $40. Why the huge difference? And is the cheaper one really the same?
They’re the same medicine - just cheaper
Generic drugs aren’t knockoffs. They’re not cheaper because they’re weaker or made in a basement. They contain the exact same active ingredient, in the same strength, and work the same way in your body as the brand-name version. The FDA requires them to match the brand in dosage, safety, effectiveness, route of administration, and stability. If your doctor prescribes atorvastatin, the generic for Lipitor, it lowers your cholesterol just as effectively. Same pill. Same result. Just a fraction of the cost.
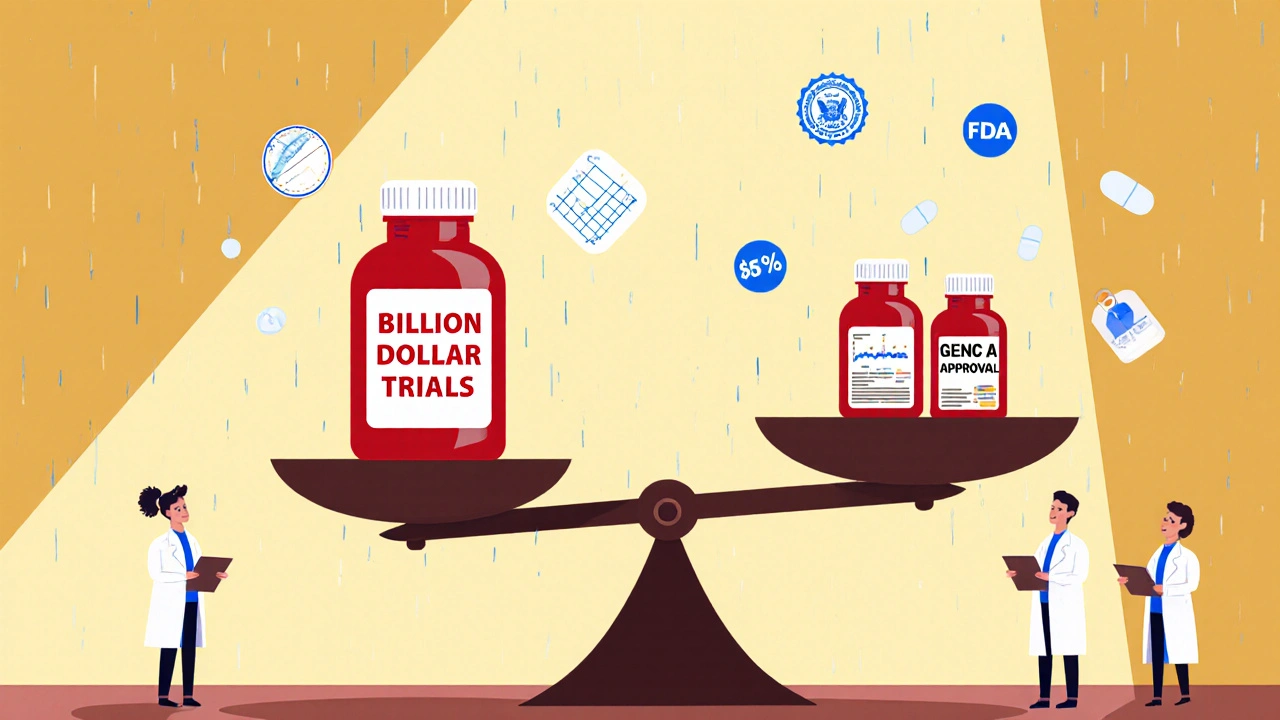
The reason generics cost so much less isn’t because they’re inferior - it’s because they don’t have to repeat the billion-dollar clinical trials the original company paid for. When a brand-name drug’s patent expires, other manufacturers can apply for approval through a faster, cheaper process called an Abbreviated New Drug Application (ANDA). All they have to prove is that their version behaves the same in your body - meaning the amount of drug absorbed and how fast it gets there falls within 80-125% of the brand’s performance. That’s the FDA’s bioequivalence standard. It’s strict. It’s science-backed. And it’s why 90% of all prescriptions filled in the U.S. in 2024 were generics.
How much cheaper are generics?
On average, generics cost 79% to 85% less than their brand-name counterparts. That’s not a guess. It’s what the FDA and independent research groups like AccessibleMeds and Tebra found in 2025 surveys. For example, if a brand-name blood pressure pill costs $150 a month, the generic version likely costs $25-$30. Over a year, that’s $1,500 saved. For people managing chronic conditions - diabetes, high cholesterol, thyroid issues - that adds up fast.
But here’s the twist: the price doesn’t stay the same forever. Once the first generic hits the market, prices drop by about 10%. With two or three generic makers competing, prices fall to 60-70% of the original. When five or more companies start making it? Prices often drop below 50% of the brand’s original cost. That’s why some generics get cheaper every year - even if the brand stays the same price.
Take Nexavar, a cancer drug. When the first generic version arrived in 2022, the manufacturer, Bayer, dropped its list price by 50% the next year. Why? Because they knew they couldn’t compete on price. So they cut their own price to hold onto some market share. That’s not common - but it’s happening more. Brand companies are learning that if they don’t lower prices before generics arrive, they’ll lose almost everything.
Why do people still choose brand-name drugs?
Even though 84% of Americans believe generics are just as effective, 62% still trust brand-name drugs more. Why? It’s not science. It’s psychology. You’ve seen the ads. You know the name. The brand feels familiar. The generic? It looks different. Maybe the pill is a different color or shape. Maybe the label doesn’t say the name you recognize.
And then there’s cost pressure. A 2025 survey found that 63% of people choose generics because they can’t afford the brand. Only 15% choose them because they believe they’re equally good. That tells you something: most people aren’t switching out of confidence - they’re switching out of necessity.
But here’s the good news: if your insurance plan has a tiered system, generics are almost always in the lowest cost tier. You pay less at the pharmacy counter. Your deductible gets used slower. Your out-of-pocket costs stay lower. And if you’re on Medicare, the Inflation Reduction Act will cap your insulin costs at $35 a month starting in 2025 - and that cap applies to generics too.
What about brand-name drug prices?
It’s easy to think brand-name drugs are getting more expensive every year. But the data says otherwise. In 2024, the average net price (after discounts and rebates) for brand-name drugs actually fell for the seventh year in a row. How? Because manufacturers are giving bigger discounts to insurers and pharmacy benefit managers to stay on formularies. The list price - the one you see on the billboard - might go up. But what you actually pay? Often less.
Still, some brands keep raising prices. Revcovi, a rare disease drug, increased its list price by 4.5% in early 2025. Why? Because there’s almost no competition. Only one company makes it. No generics. No alternatives. So they can charge what they want. That’s the exception - not the rule. But it’s a reminder: without competition, prices can stay high.
The U.S. spends way more on brand-name drugs than other countries - but that’s misleading. Why? Because in the U.S., 90% of prescriptions are generics. In countries like Canada or Germany, generics make up only 60-70% of prescriptions. So when people say “U.S. drug prices are the highest,” they’re usually comparing brand-name prices alone - ignoring the fact that Americans pay far less overall because generics are so cheap.
When you shouldn’t switch to generic
Most of the time, switching is safe and smart. But there are a few exceptions. For drugs with a narrow therapeutic index - meaning the difference between a helpful dose and a harmful one is very small - doctors may recommend sticking with the brand. Examples include warfarin (a blood thinner), levothyroxine (for thyroid), and some anti-seizure medications like phenytoin.
Why? Because even tiny differences in how the drug is absorbed can matter. Your doctor might prefer you stay on the same version - brand or generic - to keep your levels stable. If you’re on one of these, don’t switch without talking to your provider. But even here, many patients do fine on generics. It’s not a hard rule. It’s a cautious approach.
What about biosimilars?
Biosimilars are the next frontier. They’re not generics - they’re copies of complex biologic drugs, like those used for rheumatoid arthritis, cancer, or Crohn’s disease. Unlike small-molecule generics, biosimilars aren’t exact copies. They’re highly similar. But they still cut costs by 15-35%. And they’re growing fast. In 2024, biosimilars saved the U.S. healthcare system an estimated $15 billion. Expect that number to rise as more biologics lose patent protection.

How to get the best price
Always ask if a generic is available. Don’t assume your doctor automatically prescribes it. Some still default to brand names out of habit.
Use pharmacy discount cards. GoodRx, Blink Health, and others often list generics for under $10 - even when insurance doesn’t cover them.
Check your plan’s formulary. Some insurers have preferred generics. Others charge more for certain brands even if a generic exists.
Ask about 90-day supplies. Many generics are cheaper when bought in bulk. A 90-day supply can cost less than two 30-day fills.
And if you’re on Medicare Part D, remember: your out-of-pocket costs are capped at $2,000 a year starting in 2025. That includes both brand and generic drugs. So using generics helps you hit that cap slower - and keeps you protected longer.
Bottom line: Save money, get the same results
Generic drugs are not second-rate. They’re the same medicine, made to the same standards, at a fraction of the cost. Since 2019, Americans have saved over $6 billion on generic drugs - even as more people used them. That’s not a fluke. It’s the result of smart policy, fierce competition, and proven science.
If you’re paying hundreds a month for a prescription, ask your pharmacist or doctor: “Is there a generic?” The answer might save you thousands.
Are generic drugs as effective as brand-name drugs?
Yes. Generic drugs must meet the same FDA standards as brand-name drugs. They contain the same active ingredient, work the same way in your body, and are held to the same quality, purity, and strength requirements. The FDA requires them to be bioequivalent - meaning they deliver the same amount of medicine into your bloodstream at the same rate as the brand. Thousands of studies and real-world use confirm they work just as well.
Why do generics cost so much less?
Generics don’t have to repeat expensive clinical trials. When a brand-name drug’s patent expires, other companies can apply for approval using a faster process called an ANDA. They only need to prove their version works the same way in the body - not that it cures the disease from scratch. That cuts development costs dramatically. Plus, once multiple companies start making the same drug, competition drives prices down - sometimes by 80% or more.
Can I switch from a brand-name drug to a generic?
In most cases, yes. For the vast majority of medications - like blood pressure pills, antidepressants, or antibiotics - switching is safe and common. But for drugs with a narrow therapeutic index - such as warfarin, levothyroxine, or certain seizure medications - your doctor may recommend staying on the same version (brand or generic) to avoid small changes in how your body absorbs the drug. Always talk to your provider before switching.
Do generics have the same side effects?
Yes. Since generics contain the same active ingredient and work the same way, their side effect profile is identical to the brand-name version. The inactive ingredients - like fillers, dyes, or coatings - may differ slightly, which could cause rare allergic reactions in sensitive individuals. But these are uncommon and not related to the drug’s effectiveness. If you notice a change in side effects after switching, tell your doctor - but it’s not because the generic is weaker or different.
Why do generics look different from brand-name drugs?
By law, generic drugs can’t look exactly like the brand-name version - that would violate trademark rules. So they may be a different color, shape, or size. But the active ingredient is identical. The difference is only in appearance, not effect. If you’re used to a certain pill shape and find a new one, check the label to confirm it’s the same medication. Your pharmacist can help you verify this.
Are all generic drugs made in the same places as brand-name drugs?
Yes. Generic drugs are made in the same type of facilities as brand-name drugs - many are even made by the same companies. The FDA inspects all manufacturing sites, whether they produce brand or generic drugs. In fact, over half of all generic drugs sold in the U.S. are made by companies that also make brand-name drugs. The difference isn’t where they’re made - it’s who pays for the research.
Will my insurance cover generics?
Almost always. Insurance plans encourage generics because they’re cheaper. Most plans have lower copays for generics - sometimes as low as $5 or $10. Some even require you to try the generic first before covering the brand. If your plan doesn’t cover a generic, ask your pharmacist about discount programs like GoodRx, which often offer prices lower than your insurance copay.
Can I ask my doctor to prescribe a generic?
Absolutely. You have the right to ask. Many doctors automatically prescribe generics, but if yours doesn’t, just say: “Is there a generic version available for this?” or “Would a generic work for me?” Most doctors are happy to switch - it saves you money and doesn’t change your care. Only in rare cases (like narrow therapeutic index drugs) might they prefer the brand.
What to do next
If you’re taking a brand-name drug and paying more than $50 a month, check if a generic exists. Ask your pharmacist - they can tell you instantly. Use a discount app like GoodRx to compare prices. If your insurance doesn’t cover it, the cash price might still be lower than your copay.
Don’t assume you need the brand. Don’t assume the generic is worse. The data is clear: generics deliver the same results at a fraction of the cost. And in a system where healthcare spending is under pressure, they’re one of the few things that actually make care more affordable - without sacrificing quality.






8 Comments
Man, I wish more people knew this. My dad’s on a generic statin and saves like $180 a month. He used to freak out about the pills looking different, but after six months, his numbers are better than when he was on Lipitor. Same drug. Same results. Just no corporate logo on it. 🤷♂️
Let’s be real - the FDA’s bioequivalence standard is a joke. 80-125%? That’s a 45% swing. If your blood pressure med is 10% under or 20% over, you’re not ‘equivalent,’ you’re playing Russian roulette with your arteries. And don’t even get me started on the fact that 60% of generics are made in India and China - places where inspections are a suggestion, not a law. This isn’t science. It’s capitalism with a Band-Aid.
Actually, the data is misleading. The 90% generic adoption rate is a function of insurance coercion, not consumer preference. PBMs incentivize generics through rebate structures that penalize prescribers who choose brands. This isn’t market efficiency - it’s regulatory capture. And the ‘cost savings’ are illusory because the real cost is shifted to patient adherence: non-brand pills have higher discontinuation rates due to psychological aversion and inconsistent inactive ingredients. The system isn’t saving money - it’s optimizing for profit margins, not outcomes.
U.S. generics are the only reason we’re not all broke. Other countries? They pay 3x for the same meds because they don’t have competition. We’ve got 12 companies making metformin - in Texas, Florida, even Ohio. Meanwhile, Germany still lets pharma jack up prices because they’re scared of generics. America wins because we let free markets work. Stop whining about pill colors and thank the FDA for not being European.
GENERIC = WINNER 🏆💸 My insulin is $35 now and it’s generic. I cried. My mom’s cholesterol med is $8 a month. I told her to stop buying the brand and she did. Now she’s got extra cash for tacos. 🌮❤️
wait so generics are just as good??? but my cousin swears her seizure med went weird after switching… i think the fillers are sketchy?? like why do they even use different dyes?? its like the pill is trying to be a different person
I’ve been taking generic levothyroxine for five years and my TSH is rock solid. I switched from Synthroid because my insurance wouldn’t cover it. I was nervous at first, but my doctor said the differences in inactive ingredients are negligible for most people. The key is consistency - once you find a generic that works, stick with it. Don’t keep switching brands. And yeah, the pill looks like a tiny green pebble now, but it’s still doing its job. 🤝
Let’s not romanticize generics. The fact that 63% of people use them because they can’t afford the brand - not because they believe in them - speaks volumes about the collapse of American healthcare. We’ve turned medicine into a commodity, and now we’re pretending that a $5 pill is an ethical solution to systemic failure. Biosimilars? Great. But they’re still just band-aids on a broken system. The real problem? Drug patents. The real solution? Single-payer negotiation. Not ‘use GoodRx’ - that’s just corporate gaslighting with a discount card.