
Medication Nausea Prevention Tool
Your Personalized Prevention Plan
Many people start a new medication expecting relief, only to be hit with nausea or vomiting instead. It’s not rare. In fact, medication nausea is one of the most common reasons people stop taking their prescriptions. Whether it’s an antibiotic, a painkiller, or chemotherapy, your stomach doesn’t always care about your doctor’s good intentions. The good news? You don’t have to just suffer through it. There are practical, proven ways to prevent and ease nausea from medications - and you don’t always need a prescription to do it.
Why Do Medications Make You Sick?
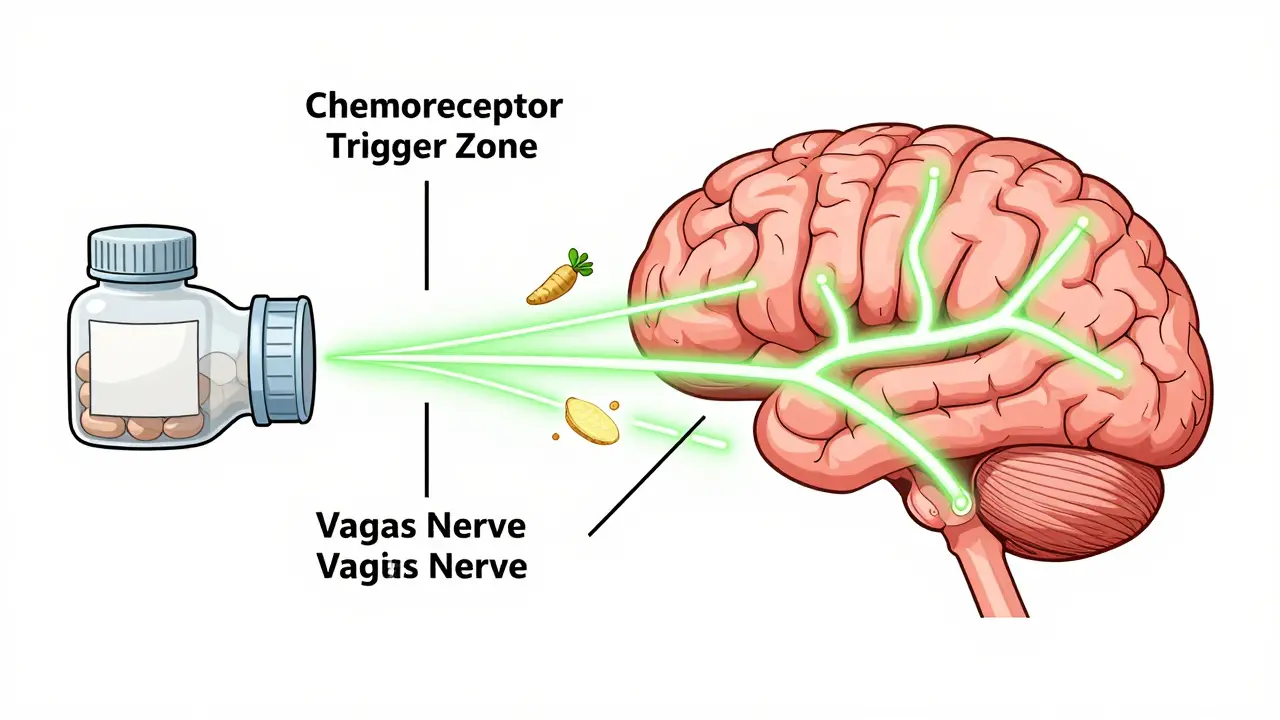
Nausea and vomiting from drugs aren’t random. They happen because of how your body reacts. Some medications irritate your stomach lining directly - think NSAIDs like ibuprofen or aspirin. Others trigger the brain’s vomiting center, often called the chemoreceptor trigger zone. This area sits near the blood-brain barrier and gets activated by chemicals in your bloodstream. Chemo drugs, for example, flood your system with toxins that this zone reads as a threat. Even SSRIs and some antibiotics can set off this alarm. Then there’s the vagus nerve, which connects your gut to your brain. Certain meds stimulate it, sending signals that make you feel queasy. And if you’ve had nausea before with a drug, your brain can start anticipating it. This is called anticipatory nausea - and it’s real. You don’t even need the drug in your system to feel sick. Just seeing the pill bottle or walking into the clinic can trigger it.Start with What’s Already in Your Kitchen
Before you reach for a pill, try simple changes. They’re low-risk, low-cost, and often surprisingly effective.- Take meds with food - unless your doctor says otherwise. Antibiotics like doxycycline, NSAIDs like naproxen, and even multivitamins are much easier on your stomach when taken with a small meal. A slice of toast, a banana, or even a spoonful of yogurt can make a big difference.
- Eat small, frequent meals - instead of three big ones. A full stomach adds pressure. Eating little bits throughout the day keeps your stomach from getting too empty or too full, both of which can worsen nausea.
- Avoid strong smells - cooking, perfumes, or even your own bathroom can set off nausea. Keep windows open. Eat cool or room-temperature foods. They have less odor than hot meals.
- Stay hydrated - but sip slowly. Chugging water can make nausea worse. Try ice chips, clear broths, or electrolyte drinks if you’re losing fluids from vomiting.
- Try ginger - it’s not just folklore. Studies and real-world reports show ginger (in tea, chews, or capsules) helps reduce nausea from chemo, motion sickness, and even pregnancy. One cancer patient on Reddit said ginger chews every two hours dropped their nausea from 8/10 to 3/10 in a day.
When Food Isn’t Enough: The Right Medicines for the Job
If lifestyle tweaks don’t cut it, there are targeted antiemetics designed to block specific nausea pathways.- 5-HT3 blockers - like ondansetron (Zofran) or granisetron (Kytril). These are the go-to for chemo and post-op nausea. They block serotonin, a chemical that triggers vomiting. Ondansetron works best when taken 30 minutes before a meal or chemo session. A 4mg tablet is standard, but some people need 8mg for full control.
- NK-1 blockers - like aprepitant (Emend) or rolapitant (Varubi). These are used for more severe cases, especially with highly emetogenic chemo. They block a different brain signal called substance P. When paired with ondansetron and dexamethasone, they boost complete nausea control to 75-85%.
- Mirtazapine - yes, an antidepressant. At low doses (15-30mg), it blocks 5-HT3 receptors and helps with nausea from chemo or surgery. It’s also a sleep aid, so it’s often taken at night.
- Low-dose tricyclics - like nortriptyline or amitriptyline. These aren’t first-line, but for chronic nausea with no clear cause (like functional dyspepsia), they can help. One study found 51% of patients had complete relief. But don’t try this without a doctor - side effects like dry mouth and dizziness can be tricky.

Timing and Dosing Matter More Than You Think
Taking a pill at the wrong time can turn a manageable side effect into a nightmare.- SSRIs like sertraline or fluoxetine? Take them at night. Dizziness and nausea often peak a few hours after dosing. Sleeping through it helps.
- Iron supplements? Take them with vitamin C-rich food (like orange juice) to help absorption - and avoid dairy. Calcium blocks iron uptake and can make stomach upset worse.
- Chemo? Start antiemetics before treatment, not after. Waiting until you feel sick means you’re already behind. Prophylaxis is key.
- Start low, go slow. If you’re on a new medication, ask your doctor about starting at half the dose for the first few days. Your body might adjust better.
What to Avoid
Some common advice actually makes things worse.- Don’t force yourself to eat - if you’re nauseated, forcing food can create a lasting aversion. Especially to your favorite foods. The American Cancer Society says 78% of patients who avoided eating favorite dishes during chemo kept their appetite longer.
- Don’t lie down right after taking pills - stay upright for at least 30 minutes. Lying flat can let stomach acid and meds irritate your esophagus.
- Don’t mix alcohol with meds - even a glass of wine with an antibiotic or painkiller can spike nausea and liver stress.
- Don’t skip doses - especially if you’re on chemo or antibiotics. Stopping because of nausea can make the underlying condition worse. Talk to your doctor instead.
Cost and Access: The Hidden Problem
Newer antiemetics like aprepitant or netupitant can cost $150-$300 per dose without insurance. That’s why 35% of patients with moderate to severe nausea cut their medication doses or stop entirely. If cost is a barrier, ask your doctor about:- Generic options - ondansetron is available as a low-cost generic.
- Patient assistance programs - drugmakers like Merck and Helsinn offer aid for branded drugs.
- Compounded alternatives - some pharmacies can make lower-cost versions of combination therapies.
When to Call Your Doctor
Not all nausea is the same. If you notice:- Vomiting for more than 24 hours
- Signs of dehydration (dark urine, dizziness, dry mouth)
- Weight loss or inability to keep down fluids
- Nausea that starts weeks after starting a new drug
- Other symptoms like fever, rash, or abdominal pain
What’s New in 2026
The field is evolving. In 2023, the FDA approved rolapitant (Varubi) for kids aged 2-17, expanding access. Hospitals are testing apps like Nausea Tracker - used by 42% of major cancer centers - to log symptoms daily and adjust treatment in real time. Behavioral therapy is also gaining ground. For anticipatory nausea, cognitive behavioral therapy (CBT) is now recommended as a standard part of care, not an afterthought.Can I use ginger with my prescription antiemetic?
Yes, ginger is generally safe to use alongside medications like ondansetron or aprepitant. Studies show it works through different pathways than drugs, so it can add extra relief. Stick to 1 gram per day in any form - tea, chews, or capsules. Avoid high doses if you’re on blood thinners.
Why does my nausea get worse at night?
Lying down slows digestion and lets stomach acid rise. If you took a medication earlier in the day, its effects may peak at night. Also, your body’s natural cortisol levels drop overnight, which can lower your nausea threshold. Try elevating your head with an extra pillow and avoid eating within 2 hours of bedtime.
Are there foods that make medication nausea worse?
Yes. Spicy, greasy, or overly sweet foods can irritate the stomach and trigger nausea. Also, strong-smelling foods like coffee, onions, or fish can set off the vomit reflex. Stick to bland, dry carbs - crackers, toast, rice, or plain pasta. Cold foods often have less odor and are easier to tolerate.
Can anxiety make medication nausea worse?
Absolutely. Stress activates the vagus nerve and increases stomach acid. If you’re anxious about taking your meds, your body may react before the drug even hits your system. Breathing exercises, meditation, or even just listening to calming music for 10 minutes before dosing can help break the cycle.
What if nothing works?
If you’ve tried food changes, ginger, timing adjustments, and standard antiemetics - and still can’t tolerate the medication - talk to your doctor. There may be an alternative drug in the same class with fewer GI side effects. Or, your dose may need to be adjusted. Never stop a prescribed medication without medical advice. Sometimes, switching from a pill to an injectable or patch can make a huge difference.






Write a comment