Alcohol & Blood Thinner Risk Calculator
Alcohol & Blood Thinner Risk Assessment
Calculate your potential INR risk based on alcohol consumption and personal factors. This tool is designed for people taking warfarin or other blood thinners. Results are for informational purposes only and should not replace medical advice.
When you're on a blood thinner like warfarin, even a simple glass of wine can become a medical decision. It’s not about giving up alcohol completely - it’s about understanding how it changes what’s happening inside your body. The real danger isn’t just getting drunk. It’s the quiet, unpredictable shift in your blood’s ability to clot - measured by something called INR.
What Is INR, and Why Does It Matter?
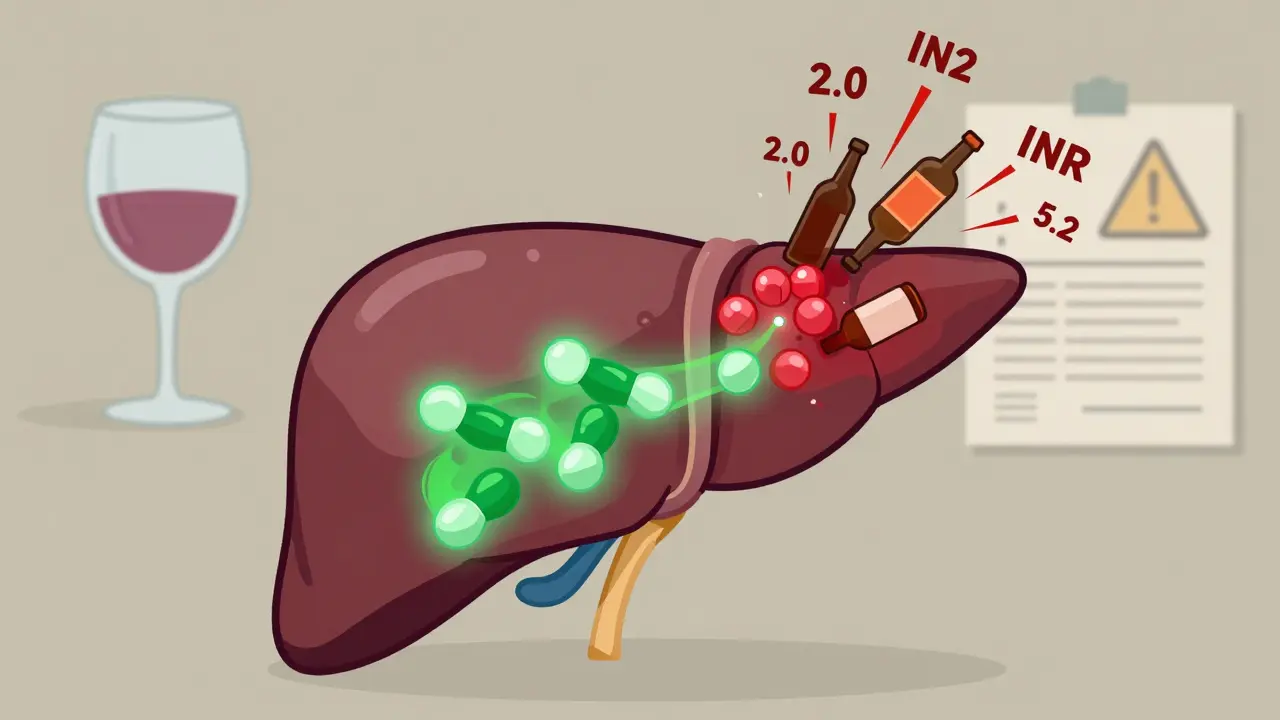
INR stands for International Normalized Ratio. It’s a number doctors use to see how long it takes your blood to clot. If you’re not on any blood thinner, your INR should be between 0.8 and 1.1. That’s normal. But if you’re taking warfarin, your target range is usually between 2.0 and 3.0. For some conditions - like a mechanical heart valve - it might go as high as 3.5. Every 0.5-point increase above your target raises your bleeding risk by 30% to 50%. So if your INR jumps from 2.5 to 3.5, you’re not just slightly more at risk. You’re entering a zone where major bleeding becomes much more likely. And when INR hits 9 or higher? That’s a medical emergency. Studies show that over a third of hospitalized patients with INR above 9 experience bleeding, and nearly one in five die from it.How Alcohol Throws Off Your INR
Alcohol doesn’t just make you feel looser - it messes with your liver, and your liver is the factory that processes warfarin. When you drink, especially in large amounts, your liver gets busy breaking down alcohol instead of warfarin. That means warfarin builds up in your blood, making your INR rise. But it’s not that simple. Sometimes, heavy drinking over days or weeks can actually lower your INR. That’s because chronic alcohol use can damage your liver so much that it stops making clotting factors properly. Suddenly, your INR drops, and you’re at risk for clots instead. This back-and-forth is why doctors hate unpredictable drinking patterns. A 2012 study found that among patients with dangerously high INR (above 9), alcohol use was one of the top three causes - right up there with kidney problems and being over 65. And here’s the kicker: if you binge drink - say, six beers in one night - your INR can spike from 2.8 to 5.2 in under 48 hours. That’s not a fluke. It’s a pattern.Warfarin vs. Newer Blood Thinners
Not all blood thinners are the same. Warfarin is old, cheap, and needs constant monitoring. Newer ones - like apixaban, rivaroxaban, and dabigatran - are called DOACs. They don’t need INR checks. They also don’t interact with alcohol the same way. DOACs are still affected by heavy drinking. Too much alcohol can irritate your stomach lining and raise your risk of bleeding, especially in the gut. But they don’t cause wild INR swings. That’s the big difference. If you’re on a DOAC, your doctor might still tell you to limit alcohol - but not because your blood test numbers will go haywire. Warfarin users, on the other hand, live by their INR numbers. One drink might be fine. Three drinks on a weekend? That’s when the phone rings. Your doctor calls because your INR is off - again.
Who’s Most at Risk?
It’s not just about how much you drink. It’s about who you are. People with certain gene variants - CYP2C9*2/*3 or VKORC1 1173G>A - break down warfarin slower. Add alcohol to the mix, and their INR spikes faster and higher. A 2015 NIH study showed these patients had a statistically higher chance of major bleeding when drinking, even at moderate levels. Older adults are also more vulnerable. Their livers don’t process alcohol as well. Their kidneys are weaker. Their bodies hold onto warfarin longer. And if they’re on other meds - like antibiotics or painkillers - the risk multiplies. Patients who’ve been on warfarin for more than a year are also at higher risk. That’s not because the drug gets stronger. It’s because their bodies are already finely tuned. A small change - like a few extra drinks - throws the whole system off balance.What Counts as Too Much?
There’s no magic number that works for everyone. But guidelines are clear: consistency beats bingeing. The British Heart Foundation says stick to no more than 14 units of alcohol per week - spread over at least three days. One unit is about half a pint of beer, a small glass of wine, or a single shot of spirits. Medical News Today defines heavy drinking as more than 14 drinks a week for men, or 7 for women. That’s not just a recommendation - it’s a red flag. Exceeding that raises bleeding risk sharply. Binge drinking - four or more drinks in one sitting - is the worst. It causes sudden INR spikes. Even if you only binge once a month, it’s enough to trigger a hospital visit. One Reddit user wrote: "My INR jumped from 2.4 to 3.8 after four glasses of wine over the weekend. My doctor said it’s common - but I had to cut back."What to Watch For: Signs of Bleeding
You don’t need to wait for an INR test to know something’s wrong. Watch for these symptoms:- Red or brown urine
- Tar-like or bright red stools
- Nosebleeds that won’t stop
- Bleeding gums when brushing your teeth
- Unusually heavy periods
- Red or brown vomit - like coffee grounds
- Unexplained bruising, especially on your arms or legs
- Severe headaches, dizziness, or confusion (could mean bleeding in the brain)
What to Do If You Drink
If you choose to drink while on warfarin, here’s how to do it safely:- Keep it consistent. Have the same amount every week - don’t save it all for Saturday.
- Avoid binge drinking at all costs. One night of heavy drinking can undo weeks of stable INR.
- Don’t mix alcohol with other medications. Even over-the-counter painkillers like ibuprofen can increase bleeding risk.
- Get your INR tested more often if you’ve had alcohol in the past week. Your doctor might want to check it sooner than usual.
- Let your doctor know if your drinking habits change. Even if you think it’s "just a little more."
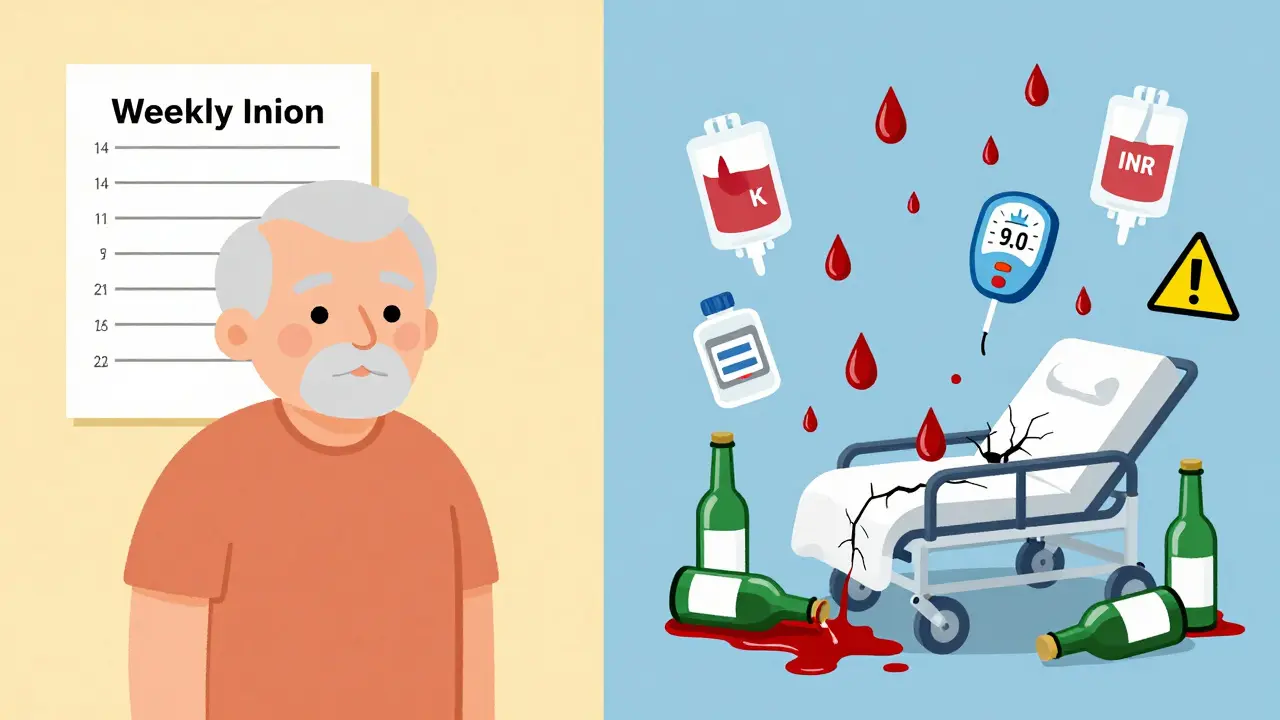
What Happens If Your INR Gets Too High?
If your INR is above 4.5, your doctor will likely pause your warfarin. If it’s above 9, you’re in danger. Vitamin K can help bring down INR - but it doesn’t work fast. Plasma transfusions, which give you fresh clotting factors, are often needed in emergencies. One study found plasma lowered INR from over 9 to 2.4 in under 24 hours. Withholding warfarin alone? Often useless. That’s why prevention matters more than treatment. Once your INR is out of control, the damage can already be done.Final Reality Check
About 30 to 40% of people on warfarin drink alcohol regularly. That’s millions of people. Most of them aren’t binge drinkers. They have a glass of wine with dinner. And they’re fine - as long as they’re consistent. The real problem isn’t alcohol. It’s inconsistency. One week you drink two glasses a day. The next week, you don’t touch it. Then you have a party and drink six. That rollercoaster is what scares doctors. You don’t have to quit. But you do have to be honest. With yourself. With your doctor. With your body. Your INR isn’t just a number on a lab report. It’s a signal - a warning that your blood is teetering on the edge. Alcohol doesn’t always tip it. But when it does, the fall can be deadly.Can I drink alcohol while taking warfarin?
Yes, but only in moderation and with consistency. The safest approach is no more than 14 units of alcohol per week, spread over three or more days. Avoid binge drinking, as it can cause dangerous spikes in your INR and increase bleeding risk.
How does alcohol affect INR levels?
Alcohol can either raise or lower your INR, depending on how much and how often you drink. Moderate, consistent drinking may slightly raise INR. Heavy or binge drinking can cause dangerous spikes, while chronic heavy use can damage your liver and lower INR, increasing clotting risk. This unpredictability makes alcohol a major concern for warfarin users.
What’s considered a safe amount of alcohol on warfarin?
No more than 14 units per week, spread over at least three days. One unit equals half a pint of beer, a small glass of wine, or a single shot of spirits. Drinking more than this, especially in one sitting, significantly increases bleeding risk.
Do newer blood thinners interact with alcohol like warfarin?
Newer blood thinners like apixaban and rivaroxaban don’t affect INR, so alcohol doesn’t cause the same lab value swings. But heavy drinking still increases bleeding risk by irritating the stomach and reducing clotting ability. Doctors still recommend limiting alcohol, even if you’re not on warfarin.
What should I do if my INR goes too high after drinking?
Call your doctor immediately. If your INR is above 4.5, they may pause your warfarin. If it’s above 9, you may need emergency treatment like vitamin K or plasma transfusion. Do not wait for symptoms - high INR can cause internal bleeding without warning.
Are there genetic factors that make alcohol more dangerous with warfarin?
Yes. People with CYP2C9*2/*3 or VKORC1 1173G>A gene variants metabolize warfarin more slowly. When combined with alcohol, these individuals face a significantly higher risk of bleeding. Genetic testing isn’t routine, but if you’ve had unexplained INR spikes, ask your doctor if genetic factors could be involved.
How often should I get my INR checked if I drink alcohol?
If you drink alcohol regularly, your doctor may recommend testing every 1-2 weeks instead of monthly. After any episode of binge drinking or increased alcohol intake, get tested within 48-72 hours to catch dangerous INR changes early.
Can I drink alcohol if I’m on a DOAC instead of warfarin?
Yes, but with caution. DOACs don’t require INR monitoring and don’t interact with alcohol the same way as warfarin. However, heavy drinking still raises your risk of stomach bleeding and other complications. Stick to moderate, consistent intake and avoid binge drinking.






8 Comments
My uncle was on warfarin for atrial fibrillation. He had one glass of red wine every night with dinner. Never missed a dose. Never spiked his INR. Consistency is everything. The second he tried to "catch up" on drinks over the weekend? Hospital. Two days. Vitamin K. Scary stuff. Don't be him.
It's worth noting that the pharmacokinetic interplay between ethanol and CYP2C9-mediated warfarin metabolism is non-linear and dose-dependent, with a pronounced first-pass effect that disproportionately impacts individuals with polymorphic variants in the VKORC1 promoter region. The clinical implication is not merely INR fluctuation-it's a disruption of hepatic cytochrome P450 homeostasis, which, when compounded by polypharmacy, can precipitate life-threatening hemorrhagic events. The notion that "moderation" is sufficient ignores the stochastic nature of drug-alcohol interactions in genetically susceptible populations.
As someone who's managed warfarin for over a decade, I'll say this: alcohol doesn't care about your intentions. It only cares about your liver's workload. If you're going to drink, treat it like insulin-same dose, same time, every day. No exceptions. No weekends off. No "I'll have two tonight because I didn't last week." That's not discipline. That's gambling with your blood.
Just wanted to say thank you for writing this. I was terrified to even mention alcohol to my doctor until I read this. Now I tell her exactly how much I drink-no shame. She adjusts my schedule accordingly. We even set up monthly check-ins if I go out. It’s not about giving up. It’s about keeping control. You got this.
Stop pretending this is complicated. Alcohol + warfarin = bad. Period. No "it depends." No "moderation." If you can’t stop drinking, get off warfarin and switch to a DOAC. Or stop being a liability to yourself and everyone around you. This isn’t a lifestyle blog. It’s a warning label.
My INR spiked to 5.1 after one cocktail at my sister’s wedding. I didn’t think it mattered. I was wrong. The ER nurse told me to stop drinking for a month and come back. I did. My INR stabilized. I still have wine once a week. But I tell my doctor. I test every two weeks. That’s the deal. No drama. Just facts.
I'm Nigerian and my dad's on warfarin. We don't drink much here but when we do, it's always with food and never more than one glass. This article made me realize how much we already do right. I'm sharing it with my cousins who live in the US. They need to hear this before they start bingeing on weekends.
My brother had an INR of 11 after a football party. They gave him plasma. He’s fine now. But he doesn’t drink anymore. Not because he’s scared. Because he realized he didn’t need it. Life’s better without the constant worry. You don’t need alcohol to have fun. You just need to be alive to enjoy it.