
When you prescribe a generic drug, you might think you’re doing the right thing-saving your patient money, following guidelines, helping the system. But in today’s legal landscape, that simple act can put your license, your practice, and your finances at risk. The truth is, physician liability for generic drug prescriptions has changed dramatically since 2011, and most doctors aren’t fully aware of how exposed they’ve become.
Why Generic Prescribing Is Now a Legal Minefield
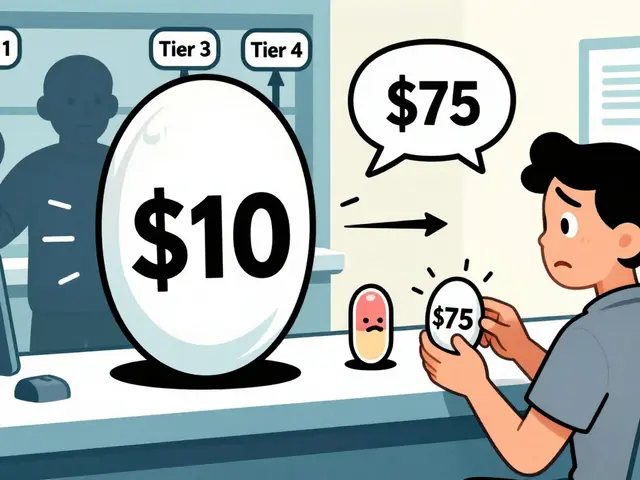
In 2011, the U.S. Supreme Court ruled in PLIVA v. Mensing that generic drug manufacturers can’t be sued for failing to update warning labels, even if their drugs cause serious harm. Why? Because federal law requires generic labels to match the brand-name version exactly. They can’t change them on their own. That ruling was reinforced in 2013 with Mutual Pharmaceutical v. Bartlett, where a woman lost 65% of her skin after taking a generic anti-inflammatory and was left permanently disfigured. She couldn’t sue the manufacturer. The court said they weren’t legally allowed to make the label safer. That left patients with nowhere to turn. And guess who they started suing instead? The doctor who wrote the prescription. According to the American Bar Association, physician-targeted lawsuits involving generic drugs jumped 37% between 2014 and 2019. These aren’t fringe cases. They’re happening in hospitals, clinics, and private practices across the country. And the numbers keep climbing.What You’re Responsible For-And What You’re Not
You’re not liable just because you prescribed a generic. But you are liable if you failed to meet the standard of care. That means three things: you had a duty to your patient, you breached that duty, and it directly caused harm. Here’s where it gets tricky: if you prescribe a drug known to cause drowsiness, and the patient crashes their car after taking it, you could be held responsible-even if it was a generic version. Why? Because the manufacturer can’t be sued for not warning about the side effect. The warning should’ve come from you. The same applies to drugs with narrow therapeutic indices-like warfarin, levothyroxine, or seizure medications. Small changes in dosage or formulation can cause serious harm. If a pharmacist switches to a generic without your knowledge, and the patient has a seizure or a stroke, you could be blamed for not preventing it.State Laws Vary-And That Makes It Worse
Forty-nine states allow pharmacists to substitute generics unless you write “dispense as written” or “do not substitute.” But here’s the catch: only 32 of those states require the pharmacist to notify you when they make the switch. In 17 states, you might never know your patient got a different version than what you prescribed. Some states have tried to fix this. Illinois courts ruled in Guvenoz v. Target Corp. that generic manufacturers still have a duty to update labels if a drug is dangerously flawed. That means doctors in Illinois might have slightly less exposure. But in most states, federal preemption rules apply-and you’re on the hook. In 2015, Alabama passed a law to block lawsuits against brand-name manufacturers for injuries caused by generics. That law was meant to protect brand companies, but it left physicians as the only possible target. It’s a legal loophole that’s costing doctors money and peace of mind.
The Rise of Defensive Prescribing
A 2022 AMA survey found that 68% of physicians feel more anxious about prescribing generics. Nearly half say they sometimes choose brand-name drugs-even when generics are cheaper and clinically equivalent-just to avoid liability. Dr. Robert Chen from Massachusetts General Hospital told colleagues he now adds 15 to 20 minutes to every visit just to document warnings. He writes out side effects by hand, explains risks verbally, and makes patients initial a form. “I don’t care if it’s inefficient,” he said. “I care if I’m sued.” This isn’t just about time. It’s about cost. Insurance premiums for primary care doctors rose 22.7% between 2013 and 2022, according to the Medical Liability Monitor. And if you don’t document your counseling properly, your insurer may charge you an extra 7.3% in premiums.How to Protect Yourself: 5 Action Steps
- Use “dispense as written” for high-risk drugs. This includes anticoagulants, thyroid meds, anti-seizure drugs, and psychiatric medications. In 32 states, this blocks substitution automatically.
- Document everything. Don’t just write “medication discussed.” Use specific language: “I discussed potential side effects of levothyroxine, including palpitations, weight loss, and insomnia. Advised patient to report chest pain or irregular heartbeat immediately.”
- Use your EHR’s built-in tools. Epic and other major systems now have mandatory fields for generic substitution counseling. Fill them out. Every time. They’re there for a reason.
- Know your state’s substitution laws. If your state doesn’t require notification, assume the pharmacist switched the drug. Be extra cautious with patients on narrow-therapeutic-index meds.
- Educate your patients. Tell them: “This is a generic version. It’s the same active ingredient, but sometimes people react differently. If you feel worse, call me right away.”

What Happens If You’re Sued?
The American College of Physicians documented 47 malpractice claims against physicians over generic drug injuries between 2011 and 2021. Twelve of those ended in settlements averaging $327,500. Most didn’t involve gross negligence. They involved missing a warning, failing to document, or assuming the pharmacist would catch it. One case involved a patient who developed Stevens-Johnson syndrome after a generic substitution. The prescribing physician had written “may substitute,” didn’t document any counseling, and didn’t know the drug was linked to severe skin reactions. The patient sued. The manufacturer couldn’t be sued. The pharmacist wasn’t liable. The doctor settled.What’s Changing Now?
The legal landscape is still shifting. In March 2023, the 9th Circuit Court ruled in Johnson v. Teva Pharmaceuticals that generic manufacturers can be held liable if they fail to update their label after the brand-name version adds a new safety warning. That’s a small crack in the preemption wall-but it’s not nationwide. The AMA is pushing for model legislation requiring pharmacists to notify physicians within 24 hours of substituting high-risk generics. Bills like this have been introduced in 18 states in 2023. But until federal law changes, you’re still the last line of defense.The Bottom Line
You didn’t ask for this. You didn’t create this system. But you’re living in it. Generic drugs are cheaper, widely used, and clinically appropriate for most patients. But the legal shield that once protected manufacturers is gone. And you’re the one now standing in front of the liability. The good news? You can protect yourself. It’s not about avoiding generics. It’s about documenting, communicating, and knowing the law. The difference between a clean record and a lawsuit might be one well-written note.Can I be sued if a patient has a bad reaction to a generic drug I prescribed?
Yes. If the generic manufacturer can’t be sued due to federal preemption (which they can’t in most cases), the patient may sue you instead. You can be held liable if you failed to warn about known side effects, didn’t document counseling, or prescribed a high-risk drug without taking proper precautions.
Does prescribing a brand-name drug protect me from liability?
Not necessarily. If you prescribe a brand-name drug and the patient takes it as written, the manufacturer can still be sued. But if the patient later gets a generic version and is harmed, you’re more likely to be targeted. Some states used to allow lawsuits against brand-name manufacturers for generic injuries, but most have passed laws blocking that. You’re still responsible for your prescribing decisions regardless of the brand.
Do I need to write “dispense as written” on every prescription?
No, but you should for drugs with narrow therapeutic indices-like warfarin, levothyroxine, phenytoin, and lithium. These drugs have small safety margins, and even minor formulation differences can cause serious harm. In many states, writing “dispense as written” prevents substitution entirely. For routine medications, it’s not required-but documentation of counseling is still essential.
What should I say to patients about generic substitution?
Say this: “This is a generic version of your medication. It has the same active ingredient and is approved by the FDA. But sometimes people react differently to generics because of inactive ingredients or how the drug is absorbed. If you notice new side effects-like dizziness, rash, or feeling worse-call me right away.” Document that conversation in your notes.
Are electronic health records helping or hurting my legal position?
They’re helping-if you use them right. Systems like Epic now have mandatory fields for documenting generic substitution counseling. If you skip them, you’re creating a gap in your defense. If you fill them out with specific details, you’re building a legal shield. The key isn’t the system-it’s how you use it.
Has the number of lawsuits against doctors for generic drugs really increased?
Yes. The American Bar Association reported a 37% increase in physician-targeted lawsuits involving generic drugs between 2014 and 2019. The Medical Risk Management, Inc. 2023 report found that physicians who document counseling reduce their liability exposure by 58%. That’s not a coincidence-it’s a pattern.



11 Comments
Just read this and my jaw dropped. I’ve been prescribing generics for years thinking I’m doing the right thing-turns out I’ve been walking through a minefield blindfolded. Thanks for laying this out so clearly. I’m already updating my templates today.
OMG this is so important!! I just started my residency and no one told me any of this!! I’m gonna start writing ‘dispense as written’ on EVERYTHING now 😅🙏
You’re all being dramatic. This is just malpractice fearmongering. If you can’t handle the legal risks, maybe don’t prescribe.
Oh wow, so the solution is to make every visit 20 minutes longer and turn every patient interaction into a legal deposition? Brilliant. Next you’ll be asking patients to sign a waiver before you hand them a Tylenol.
Actually, I think this whole thing is a corporate scam. Generic drugs are just as safe. The real problem is that big pharma doesn’t want you to save money. This ‘liability’ narrative? Totally manufactured to keep prices high.
Why are we letting foreign drug makers dictate our medical liability? This is why America needs to bring manufacturing back. No more foreign generics. No more lawsuits. Just American-made meds and American doctors who know what they’re doing.
Y’all are overcomplicating this 😊 Just talk to your patients, document like your license depends on it (it does), and stop panicking! You’re not alone in this. We’ve got this! 💪❤️
hi everyone! i just wanted to say this post made me cry a little because i’ve been doing this for 22 years and no one ever taught me about the label thing. i’m from texas and we dont even have notification laws here 😔 i’m gonna start using the epic prompts now and i’m gonna teach my med students too. you’re all doing great. love you.
But have you considered the ontological implications of pharmaceutical identity? If a generic drug is chemically identical, yet legally distinct in liability, does that not reveal a fundamental fracture in the epistemology of medical authority? The state, through preemption, has rendered the physician as the ontological anchor of pharmacological meaning - a tragic inversion of the Hippocratic ideal.
Just wanted to say… I’ve been using the Epic mandatory fields… and… it’s… actually… helped… a lot… I used to skip them… now I fill them out… every time… even for… amoxicillin… just… in case…
It’s not the law that’s flawed-it’s the entire paradigm of pharmaceutical regulation that’s been corrupted by neoliberal deregulation and the commodification of health. The Supreme Court’s rulings are symptomatic of a deeper rot in the American legal imagination-a failure to recognize the physician as a moral agent rather than a contractual intermediary. You’re not just documenting side effects-you’re resisting the erosion of professional autonomy.