Understanding Embolism
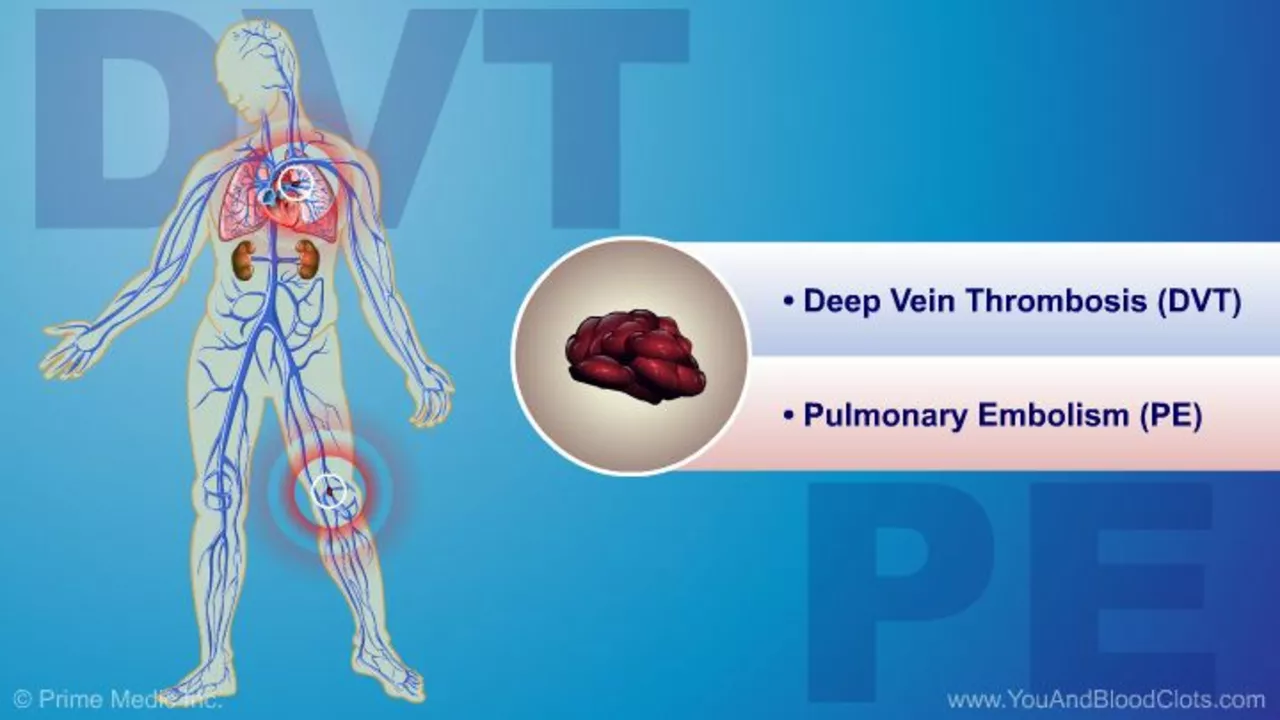
The term embolism might be relatively unfamiliar to many, but it's an important concept to understand, particularly for those living with chronic conditions like diabetes. An embolism is a sudden blockage of a blood vessel. This blockage typically occurs when a blood clot, also known as a thrombus, breaks away and travels through the blood to become lodged in a smaller vessel. This can lead to serious complications, such as stroke or heart attack.
Exploring Diabetes
Diabetes, on the other hand, is a well-known and increasingly common disease. It is a chronic condition that affects the way your body processes blood sugar, also known as glucose. The two main types of diabetes are type 1 and type 2. Type 1 diabetes is usually diagnosed in children and young adults and is a condition in which the body does not produce insulin. Type 2 diabetes is more common and occurs when your body becomes resistant to insulin or doesn't make enough insulin.
Linking Embolism and Diabetes
Now that we have a basic understanding of both embolism and diabetes, let's explore the connection between the two. Research shows that people with diabetes have an increased risk of developing blood clots, which can lead to an embolism. This is due to several factors associated with diabetes, such as high blood sugar levels, inflammation, and changes in blood flow. Additionally, certain complications of diabetes, such as damage to the blood vessels, can further increase this risk.
Recognizing the Risk Factors
Understanding the risk factors for both embolism and diabetes can help in the early detection and prevention of these conditions. For diabetes, some of the key risk factors include obesity, lack of physical activity, a family history of diabetes, and certain ethnic backgrounds. Meanwhile, the risk factors for embolism often overlap with those for heart disease and stroke, such as high blood pressure, high cholesterol, and smoking. It's important to note that having diabetes itself is a risk factor for embolism.
Preventing Complications
Prevention is always better than cure. Even though there is no surefire way to prevent diabetes or embolism, there are steps you can take to reduce your risk. These include maintaining a healthy weight, eating a balanced diet, exercising regularly, and avoiding smoking. Additionally, if you have diabetes, it's crucial to manage your blood sugar levels effectively to reduce the risk of complications, including embolism.
Managing Embolism and Diabetes Together
Living with both diabetes and an embolism can be challenging, but it's not impossible. With the right treatment plan and lifestyle changes, you can manage both conditions effectively. This may involve taking medication, adjusting your diet, incorporating physical activity into your routine, and regularly checking in with your healthcare provider. Remember, you're not alone in this journey, and there are many resources available to help you navigate these challenges.


20 Comments
The mechanistic underpinnings of hypercoagulability in diabetic cohorts are often oversimplified in popular discourse. Hyperglycemia induces endothelial dysfunction via advanced glycation end‑products, which in turn primes platelet aggregation. Moreover, the inflammatory cascade mediated by NF‑κB upregulation creates a pro‑thrombotic milieu that predisposes to embolic events. It is insufficient to attribute embolism risk solely to “high blood sugar” without acknowledging the synergistic role of dyslipidemia and hypertension. Therefore, any preventive strategy must be multidimensional, integrating glycemic control, lipid management, and antiplatelet therapy.
While the article attempts a decent overview, it conveniently neglects the nuanced pharmacodynamics of newer SGLT‑2 inhibitors, which have demonstrated a modest reduction in thrombo‑embolic incidents. One could argue that the omission is a deliberate simplification for mass appeal, but it borders on intellectual negligence. The linkage between insulin resistance and platelet hyperreactivity is far from trivial, and deserves a more rigorous exposition.
First and foremost, let me say that navigating the intersection of embolism and diabetes is like trying to read a map in a foggy storm. The blood vessels in a diabetic patient are not merely pipes; they are living tissues constantly assaulted by glucose spikes, oxidative stress, and low‑grade inflammation. These assaults gradually erode the endothelial lining, making it a perfect landing strip for rogue clots. When a thrombus finally detaches, it rides the bloodstream with a speed that would make a roller coaster jealous. If it lodges in a cerebral artery, the result is an embolic stroke, a nightmare that can strip away speech, movement, and memory. Even if it settles in a peripheral artery, the attendant ischemia can lead to gangrene, forcing amputations that change a life forever. What many people overlook is that hyperglycemia itself fuels a pro‑coagulant state by increasing fibrinogen levels and reducing natural anticoagulants like protein C. Add to that the fact that insulin resistance impairs fibrinolysis, so the body’s ability to dissolve clots is hampered. Many clinical trials now show that tight glycemic control, though challenging, does correlate with a modest decline in clot‑related events. Lifestyle interventions such as regular aerobic exercise improve endothelial nitric oxide production, which acts as a vasodilator and anti‑platelet agent. Dietary choices low in refined sugars and saturated fats further reduce the inflammatory burden that primes clot formation. From a pharmacologic perspective, agents like low‑dose aspirin, statins, and newer antiplatelet drugs provide an extra layer of protection, especially in high‑risk individuals. It is also worth noting that chronic kidney disease, a frequent companion of diabetes, amplifies the risk of both embolism and bleeding, demanding a careful balance. Patients should be educated to recognize early warning signs such as sudden numbness, chest discomfort, or unexplained shortness of breath. In summary, the connection between embolism and diabetes is a complex tapestry woven from metabolic, vascular, and inflammatory threads, and untangling it requires a holistic approach that combines medical therapy, lifestyle changes, and vigilant monitoring.
Some folks forget that the pharmaceutical lobby has a vested interest in keeping us dependent on medication, which subtly shifts the risk calculus for embolic events. The data that is publicly released is often cherry‑picked, making us question the true incidence rates. It’s worth staying skeptical of mainstream narratives.
Wow, never thought my morning coffee could be a tiny clot‑preventer 😂
It’s terrifying how a silent clot can swoop in and steal years of your life – 😢 stay proactive, friends.
Indeed, SGLT‑2 inhibitors have shown promise beyond glucose lowering; their impact on endothelial function is gaining attention. Incorporating them early could blunt the pro‑thrombotic cascade you mentioned.
Good points, just a tiny note: “hyperglycemia induces endothelial dysfunction via advanced glycation end‑products,” should be “through”. Minor edit.
Thanks for the thorough breakdown; I especially appreciated the reminder about lifestyle’s role in nitric oxide production.
Reading this feels like watching a thriller where the villain is a sugar molecule.
Exactly, the plot twist is that the hero’s weapon is a balanced diet and regular walks.
From a clinical standpoint, the American Diabetes Association recommends annual screening for peripheral arterial disease in patients with longstanding diabetes, precisely because of the heightened embolic risk. Additionally, integrating a multidisciplinary care team-including endocrinologists, cardiologists, and vascular surgeons-optimizes outcomes. Patients should also be counseled on the signs of acute limb ischemia and instructed to seek immediate care if symptoms arise.
While the guidelines are well‑intentioned, they often get lost in translation to primary‑care settings, leading to delayed referrals and suboptimal management.
Oh great, another “keep‑it‑simple” post that pretends we can solve complex coagulopathy with a single salad. Newsflash: biology isn’t a Pinterest board.
Indeed!!!; It’s refreshing to see someone call out the oversimplification!!!; Let’s remember that real progress comes from nuanced research, not buzzwords!!!
Respectfully, the assertion that “high blood sugar alone” drives embolism disregards the extensive literature on multifactorial etiology. 📚 Moreover, the phrase “blood sugar levels” should be singular when referring to the metric, i.e., “blood glucose level.” Precision matters.
Absolutely, precision in language reflects precision in care – I’ll make sure to adopt the corrected terminology moving forward.
Adding to that, cultural dietary patterns influence glycemic spikes, so public health messages must be tailored, not one‑size‑fits‑all.
Just a quick note: the term “embolism” derives from the Greek “embolós,” meaning “to throw in,” which nicely captures the concept of a clot being thrown into the circulation.
Nice fact its good to know about origins