Antibiotic Selection Tool
Select Your Scenario
Recommendation Results
Select your scenario and click "Find Best Antibiotic" to see recommendations
Quick Takeaways
- Keftab (Cephalexin) is a first‑generation cephalosporin best for skin, bone and urinary infections.
- It shares a beta‑lactam core with penicillins but resists many common beta‑lactamases.
- Alternatives such as amoxicillin, doxycycline, clindamycin and azithromycin cover overlapping but distinct bacterial spectrums.
- Key decision factors: infection site, susceptibility patterns, patient allergies, and dosing convenience.
- For community‑acquired infections without penicillin allergy, Cephalexin often offers a simpler, well‑tolerated option.
What is Keftab (Cephalexin)?
When you see the brand name Keftab is the Australian trade name for the generic antibiotic Cephalexin, think of a white‑pill that belongs to the first‑generation cephalosporin family. Cephalexin was first approved by the U.S. Food and Drug Administration (FDA) in 1979 and has since become a staple for doctors treating mild to moderate bacterial infections.
Cephalexin works by interrupting cell‑wall synthesis in susceptible bacteria, leading to rapid bacterial death. Its beta‑lactam ring is similar to that of penicillins, but chemical tweaks give it extra stability against many beta‑lactamases that would otherwise break down penicillin drugs.
How Cephalexin Works: The Science in Simple Terms
The drug targets the enzyme transpeptidase, which links peptidoglycan strands in the bacterial cell wall. By binding to this enzyme, Cephalexin prevents the final cross‑linking step, leaving the wall weak and leaky. Without a sturdy wall, bacteria cannot survive the osmotic pressure of their environment and burst open.
Because the mechanism relies on a structure common to many Gram‑positive bacteria, Cephalexin is especially potent against Staphylococcus aureus (non‑MRSA), Streptococcus pyogenes, and certain Enterococcus species. Its activity against Gram‑negative organisms is modest, which is why doctors often pair it with other agents when a broader spectrum is needed.
When Doctors Prescribe Keftab
Typical indications include:
- Uncomplicated skin and soft‑tissue infections (e.g., cellulitis, impetigo).
- Bone infections like osteomyelitis caused by susceptible organisms.
- Urinary tract infections (UTIs) where Escherichia coli is known to be sensitive.
- Dental abscesses after dental extraction.
- Prophylaxis before certain surgical procedures.
The usual adult dosage ranges from 250mg to 1g taken 2‑4 times daily, depending on infection severity. Children receive weight‑based dosing, generally 25‑50mg/kg per day divided into multiple doses.
Key Alternatives to Cephalexin
Not every infection fits Cephalexin’s profile. Below are four widely used alternatives, each with distinct strengths and weaknesses.
Amoxicillin
Amoxicillin is a broad‑spectrum penicillin that covers many of the same Gram‑positive bugs as Cephalexin but also hits a few additional Gram‑negative organisms like Haemophilus influenzae. It’s often the first choice for otitis media, sinusitis, and community‑acquired pneumonia.
Doxycycline
Doxycycline is a tetracycline antibiotic prized for its oral convenience (once‑daily dosing) and activity against atypical bacteria, such as Mycoplasma and Chlamydia, plus some MRSA strains. It’s a go‑to for travel‑related diarrhea and certain tick‑borne infections.
Clindamycin
Clindamycin is a lincosamide that penetrates bone and abscesses very well. It’s an excellent fallback for patients allergic to beta‑lactams, but it carries a higher risk of Clostridioides difficile colitis.
Azithromycin
Azithromycin is a macrolide known for its long half‑life, allowing a 5‑day course to replace a typical 7‑10‑day regimen. It works nicely for atypical pneumonia and certain sexually transmitted infections, yet resistance among Streptococcus pneumoniae has risen sharply.
Side‑Effect Profiles at a Glance
All antibiotics can cause gastrointestinal upset, but the frequency and severity differ. Below is a quick reference:
- Keftab (Cephalexin): nausea (10‑15%), mild diarrhea (5‑10%), rare rash.
- Amoxicillin: similar GI upset, higher chance of allergic rash (up to 10%).
- Doxycycline: photosensitivity, esophageal irritation, possible yeast infections.
- Clindamycin: higher incidence of C.difficile infection (up to 5%).
- Azithromycin: generally well‑tolerated, but can cause QT‑prolongation in susceptible patients.
Comparison Table: Cephalexin vs. Common Alternatives
| Attribute | Cephalexin (Keftab) | Amoxicillin | Doxycycline | Clindamycin | Azithromycin |
|---|---|---|---|---|---|
| Drug class | First‑gen cephalosporin | Penicillin | Tetracycline | Lincosamide | Macrolide |
| Typical spectrum | Gram‑positive, limited Gram‑negative | Gram‑positive + some Gram‑negative | Atypicals, some MRSA, Gram‑negative | Gram‑positive (incl. beta‑lactam‑allergic) | Gram‑positive, atypicals |
| Standard adult dose | 250mg-1g q6‑8h | 500mg q8h | 100mg BID | 300mg q6h | 500mg day1, then 250mg daily x4 days |
| Common side effects | Nausea, mild diarrhea | Rash, GI upset | Photosensitivity, esophagitis | C.difficile risk | QT prolongation, mild GI |
| Penicillin allergy? | Cross‑reactivity ≈ 5% | Contraindicated | Safe | Safe | Safe (but watch for cross‑reactivity with macrolide‑allergic) |
| Pregnancy category | B | B | D (avoid unless needed) | B | D (late pregnancy caution) |
How to Choose the Right Antibiotic
Think of the selection process as a checklist rather than a guess. Ask yourself:
- What is the likely pathogen? Culture results are gold, but empiric choices rely on common culprits for the infection site.
- Is the patient allergic to beta‑lactams? A documented penicillin allergy pushes you toward clindamycin or a macrolide.
- Does the infection involve bone or deep tissue? Drugs that penetrate well (Cephalexin, Clindamycin) are preferred.
- Are there local resistance patterns? In regions with high macrolide resistance, azithromycin loses appeal.
- What dosing schedule fits the patient? Once‑daily agents (Doxycycline, Azithromycin) improve adherence for busy adults.
- Any special populations? Pregnancy, renal impairment, and children each shift the risk‑benefit balance.
When the infection is a straightforward skin infection in a non‑allergic adult, Cephalexin often wins because it’s cheap, well‑tolerated, and hits the usual suspects. If the same patient has a penicillin allergy, clindamycin becomes the next logical step.
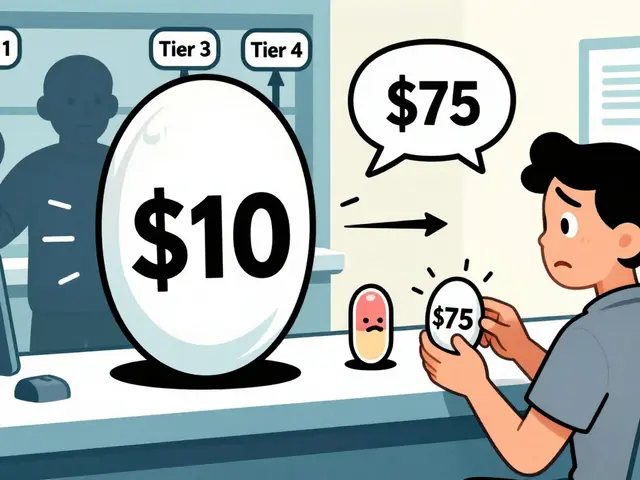
Special Considerations for Australian Patients
Australian Therapeutic Guidelines (2024 edition) list Cephalexin as a first‑line oral option for uncomplicated cellulitis and mild osteomyelitis. The government PBS subsidises Cephalexin, Amoxicillin, and Doxycycline, but not clindamycin or azithromycin unless a specialist writes the script. That cost difference can influence prescribing in a public health setting.
The rise of community‑acquired MRSA in parts of Western Australia has prompted clinicians to add coverage with doxycycline or clindamycin when MRSA is suspected. However, susceptibility testing still shows that about 85% of MSSA isolates remain fully sensitive to Cephalexin, keeping it in the frontline toolbox.
Potential Pitfalls & How to Avoid Them
- Cross‑reactivity mistake: Many prescribers assume a 10% cross‑reactivity between penicillins and cephalosporins. Modern data suggest it’s closer to 1‑2% for first‑generation agents like Cephalexin, so an uncomplicated penicillin allergy may not rule it out.
- Skipping the loading dose: For severe skin infections, an initial 1g dose of Cephalexin can achieve therapeutic levels faster.
- Ignoring renal function: Cephalexin is renally cleared; dosing should be halved for eGFR <30mL/min.
- Overlooking drug interactions: Doxycycline chelates with calcium supplements, reducing absorption-take it on an empty stomach.
FAQs
Can I take Keftab if I’m allergic to penicillin?
Most people with a mild penicillin allergy can safely use Cephalexin because the cross‑reactivity rate is low (about 1‑2%). However, if you’ve had anaphylaxis, avoid it and choose a non‑beta‑lactam like clindamycin.
How long does a typical Cephalexin course last?
For uncomplicated skin infections, 7‑10days is standard. Bone infections may require 4‑6weeks of therapy, depending on response and imaging.
Is Cephalexin effective against MRSA?
Most community‑acquired MRSA strains are resistant to Cephalexin. If MRSA is suspected, doctors usually add doxycycline or clindamycin instead.
Can I take Cephalexin with alcohol?
There’s no direct chemical interaction, but both alcohol and Cephalexin can irritate the stomach. It’s safer to limit alcohol until the course ends.
What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s almost time for the next one. In that case, skip the missed pill-don’t double up.
Bottom Line
If you need an oral antibiotic for a typical skin, bone, or urinary infection and you don’t have a severe beta‑lactam allergy, Cephalexin (Keftab) is a solid, affordable choice. When the infection involves atypical bacteria, MRSA, or when the patient can’t tolerate beta‑lactams, alternatives like doxycycline, clindamycin or azithromycin fill the gaps.
Always pair the drug choice with a quick look at local resistance patterns, patient history, and practical dosing considerations - that’s the shortcut to successful treatment without unnecessary side effects.


19 Comments
Cephalexin is a solid choice for uncomplicated skin infections, especially when you need something affordable and easy on the stomach.
That tool looks pretty handy – you can just pick skin, no allergy, and it flashes Cephalexin instantly. Makes the whole decision process feel less like guesswork.
One cannot help but notice the sleekness of the UI, yet the underlying pharmacology remains as drearily conventional as ever-another glorified spreadsheet of old‑school guidelines.
Permit me to elaborate upon the nuanced considerations that, when duly contemplated, elevate this discourse beyond mere tabular comparisons. First, the pharmacokinetic profile of cephalexin, a first‑generation cephalosporin, is distinguished by its rapid oral absorption, achieving peak plasma concentrations within one hour of ingestion, thereby furnishing prompt therapeutic levels. Second, its renal excretion mandates dose adjustments in the context of diminished glomerular filtration, a point often under‑emphasized in cursory summaries. Third, the specter of cross‑reactivity with penicillin allergy, historically exaggerated to ten percent, has been refined by contemporary immunologic studies to a modest one to two percent, an insight that has implications for prescribing in allergy‑laden patients. Fourth, while the antimicrobial spectrum is robust against gram‑positive cocci, its activity against gram‑negative bacilli is limited, necessitating adjunctive agents if broader coverage is required. Fifth, the drug’s safety profile is commendably benign, with adverse events comprising mild gastrointestinal upset in a minority of cases, and a negligible incidence of serious reactions such as Stevens‑Johnson syndrome. Sixth, the cost‑effectiveness of cephalexin cannot be overstated; in most health systems it remains a generic that imposes minimal financial burden on patients. Seventh, the drug’s bone penetration, quantified by a tissue‑to‑plasma ratio of approximately 0.1 to 0.2, renders it an acceptable option for uncomplicated osteomyelitis, though not the gold standard for deep‑seated infections. Eighth, its utility in pregnancy is affirmed by its category B classification, a reassurance for clinicians navigating the delicate balance of maternal‑fetal safety. Ninth, the emergence of community‑acquired methicillin‑resistant Staphylococcus aureus (CA‑MRSA) in certain locales attenuates its utility, prompting consideration of agents such as doxycycline or clindamycin where MRSA prevalence exceeds twenty percent. Tenth, pediatric dosing, typically articulated as 25 to 50 milligrams per kilogram per day divided into four doses, affords flexibility across the spectrum of childhood weight ranges. Eleventh, the interaction profile is sparse, with negligible cytochrome P450 involvement, thereby minimizing the potential for clinically significant drug‑drug interactions. Twelfth, the advent of fixed‑dose combination tablets, albeit limited, offers convenience for patients requiring concomitant therapies. Thirteenth, the evolution of resistance patterns underscores the necessity of periodic local antibiograms to inform empiric choices. Fourteenth, stewardship programs frequently prioritize cephalexin as a first‑line agent for uncomplicated infections, reflecting its favorable risk‑benefit ratio. Fifteenth, the patient‑centric advantage of a thrice‑daily regimen, compared with more frequent dosing schedules of alternative agents, cannot be ignored when adherence is a paramount concern. In summation, while the comparison chart succinctly captures the essential data, the clinical milieu demands a deeper, multifactorial appraisal that integrates pharmacology, patient characteristics, epidemiology, and health‑economic considerations.
I appreciate the way the tool factors in renal impairment – dose tweaking is crucial, and many apps overlook that detail.
For a patient who’s pregnant and allergic to penicillin, the recommendation of clindamycin feels spot‑on; it’s safe and reaches the placenta well.
The script does its job, but the lack of a warning about C. difficile with clindamycin is a glaring omission.
Nice layout, quick results – I’d love to see a “download PDF” button for the recommendation.
The bone infection option is helpful; I didn’t realize Cephalexin had decent bone penetration.
🚀 Love that the tool handles pediatric dosing automatically – saves a lot of mental math, especially when juggling weight‑based calculations. 📊
Mate this thing is ace for quick picks but dont trust it 4 serious infections – always double check with a doc.
Technically, the “cross‑reactivity ≈ 5%” line is inaccurate; peer‑reviewed data places it at 1‑2 % for first‑generation cephalosporins, so the tool’s wording should be corrected.
In my experience, the Australian PBS subsidy actually excludes clindamycin unless a specialist writes it – that’s a major cost factor that isn’t mentioned.
👏 Great job on adding the pregnancy category B note – it reassures both clinicians and expectant mothers that Cephalexin is generally safe. 😊
The side‑effect table is a nice quick reference, though it could benefit from a column on severity grading.
One has to wonder why the developers chose to omit any mention of the growing resistance to macrolides in Streptococcus pneumoniae – perhaps a deliberate attempt to downplay the limitations of azithromycin? It’s almost as if they’re trying to push a certain narrative about certain drug classes, which is suspicious. Moreover, the tool’s insistence on recommending Cephalexin for “most infections” seems overly simplistic, ignoring the nuanced epidemiology of local resistance patterns. It feels like they’re giving a one‑size‑fits‑all answer to a complex problem, and that is exactly the kind of oversimplification that can lead to misuse of antibiotics and, ultimately, increased resistance. Not to mention the lack of any disclaimer about the potential for allergic cross‑reactivity in patients with a vague “penicillin allergy” history – it’s like they’re assuming all clinicians will know the fine print. This is why I always double‑check everything against up‑to‑date institutional guidelines.
Overall, the tool offers a clear visual hierarchy; the color‑coded recommendation panel makes it easy to spot the primary drug at a glance, which is especially helpful in fast‑paced clinical settings.
Honestly, it feels a bit too sterile – a dash of personality wouldn’t hurt.
Great resource.