Serotonin Syndrome Risk Calculator
Assess Your Risk
This tool estimates your risk of serotonin syndrome when taking antiemetics with serotonergic medications. Based on FDA guidelines and clinical evidence.
Every year, millions of people get nausea and vomiting treated with antiemetics like ondansetron (Zofran). Many of these same people are also taking antidepressants-SSRIs like sertraline or fluoxetine-to manage anxiety, depression, or OCD. What happens when these two types of drugs meet in the body? The answer isn’t simple. While most people take them together without issue, a small but dangerous risk exists: serotonin syndrome.
What Is Serotonin Syndrome?
Serotonin syndrome isn’t just a side effect. It’s a medical emergency caused by too much serotonin activity in your brain and nervous system. This isn’t about having too much serotonin in your blood-it’s about receptors getting overstimulated. The condition was first noticed in the 1960s when doctors saw patients on MAOIs and SSRIs develop sudden confusion, shaking, and high fever. Today, we know it can happen with any combination of drugs that boost serotonin levels-whether by increasing its release, blocking its breakdown, or preventing its reabsorption.It’s rare. But when it happens, it can be deadly. The symptoms come on fast-often within hours. You might feel restless, start sweating heavily, have muscle twitches, or feel like your heart is racing. More serious signs include high blood pressure, fever over 101°F, confusion, or even seizures. If you’re on an SSRI and get an ondansetron shot for nausea after surgery, and then suddenly feel off, this is the red flag you need to recognize.
Why Do Antiemetics Even Matter?
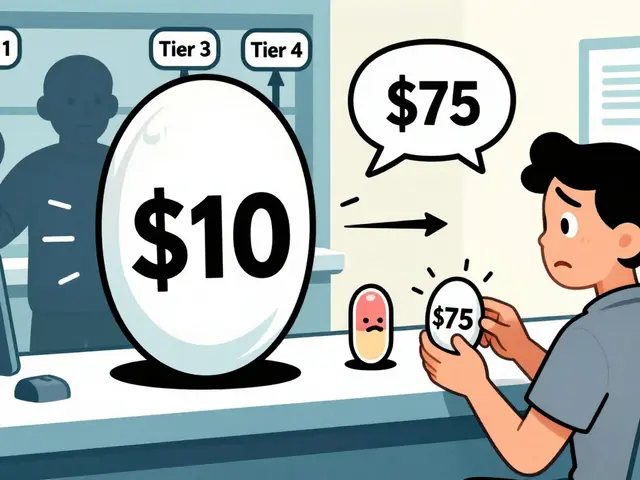
Most people assume antiemetics like ondansetron are safe because they block serotonin-not activate it. That’s true for the 5-HT3 receptors in your gut, which is why they work so well for chemo nausea or morning sickness. But drugs don’t always behave the way we expect. Research shows that ondansetron and similar drugs may have weak, off-target effects on other serotonin pathways. In lab studies, they’ve been shown to slightly interfere with serotonin reuptake, just enough to matter when combined with stronger drugs like SSRIs.Metoclopramide (Reglan), another antiemetic, is a different story. It’s not primarily a serotonin drug, but it has mild serotonin reuptake-blocking properties. Between 2004 and 2018, the FDA logged 17 confirmed cases of serotonin syndrome linked to metoclopramide used with SSRIs. Aprepitant (Emend), used for severe nausea in cancer patients, doesn’t directly affect serotonin-but it slows down how fast your liver breaks down SSRIs. That means more SSRI stays in your system, increasing the chance of overload.
Even if the direct risk is low, the problem is how often these drugs are mixed. In 2022, over 22 million ondansetron prescriptions were filled in the U.S. Nearly 40% of those were given to people already on an SSRI. That’s a huge pool of potential interactions.
Who’s Most at Risk?
It’s not just about what drugs you take-it’s about who you are. Older adults, especially those over 65, are far more vulnerable. Data shows they make up over 40% of serotonin syndrome cases involving ondansetron and SSRIs, even though they only represent about 19% of the population. Why? Their livers and kidneys don’t clear drugs as efficiently. Their brains are more sensitive. And they’re more likely to be on multiple medications.Genetics also play a role. About 7-10% of people of European descent are “poor metabolizers” of CYP2D6, a liver enzyme that breaks down ondansetron. If you’re one of them and you’re also on fluoxetine (a strong CYP2D6 inhibitor), your ondansetron levels can spike 2.3 times higher than normal. That’s not a small increase-it’s enough to tip the balance toward serotonin overload.
People on multiple serotonergic drugs are at highest risk. This includes anyone taking an SSRI or SNRI with tramadol, dextromethorphan (in cough syrups), triptans (for migraines), or even St. John’s wort. Add an antiemetic into that mix, and the risk compounds.
What Does the Evidence Really Say?
You’ll hear conflicting things. Some doctors say ondansetron is safe. Others say it’s a hidden danger. The truth? Most cases of serotonin syndrome involving antiemetics happen when two or more serotonergic drugs are used together. A 2022 analysis from the EMCrit Project found that 96.4% of reported cases had at least one other serotonin-boosting drug present.The FDA still says the benefits of ondansetron outweigh the risks. And they’re right-for most people. But “most” doesn’t mean “all.” Case reports are real. In one 2017 study, a 62-year-old man developed serotonin syndrome after getting ondansetron for nausea while on citalopram. He had no other risk factors. He recovered after stopping both drugs, but he spent three days in the ICU.
On patient forums like Reddit, hundreds report similar stories. People describe feeling “electric,” trembling uncontrollably, or having their heart pound after getting ondansetron during a dental visit while on an SSRI. Eleven of those cases required emergency care. These aren’t outliers-they’re warning signs.
How Do Doctors Know It’s Serotonin Syndrome?
There’s no single blood test. Diagnosis relies on recognizing the pattern. The Hunter Serotonin Toxicity Criteria is the gold standard. It looks for specific combinations of symptoms:- Serotonin agonist use + spontaneous clonus
- Serotonin agonist use + inducible clonus + agitation or diaphoresis
- Serotonin agonist use + ocular clonus + agitation or diaphoresis
- Serotonin agonist use + tremor + hyperreflexia
- Serotonin agonist use + temperature over 38°C + ocular or inducible clonus
If you meet one of these, serotonin syndrome is likely. The criteria are 84% sensitive and 97% specific-meaning they rarely miss it and rarely get it wrong. If you’re on an SSRI and get ondansetron, then develop tremors, sweating, and overactive reflexes, this is the checklist doctors use.
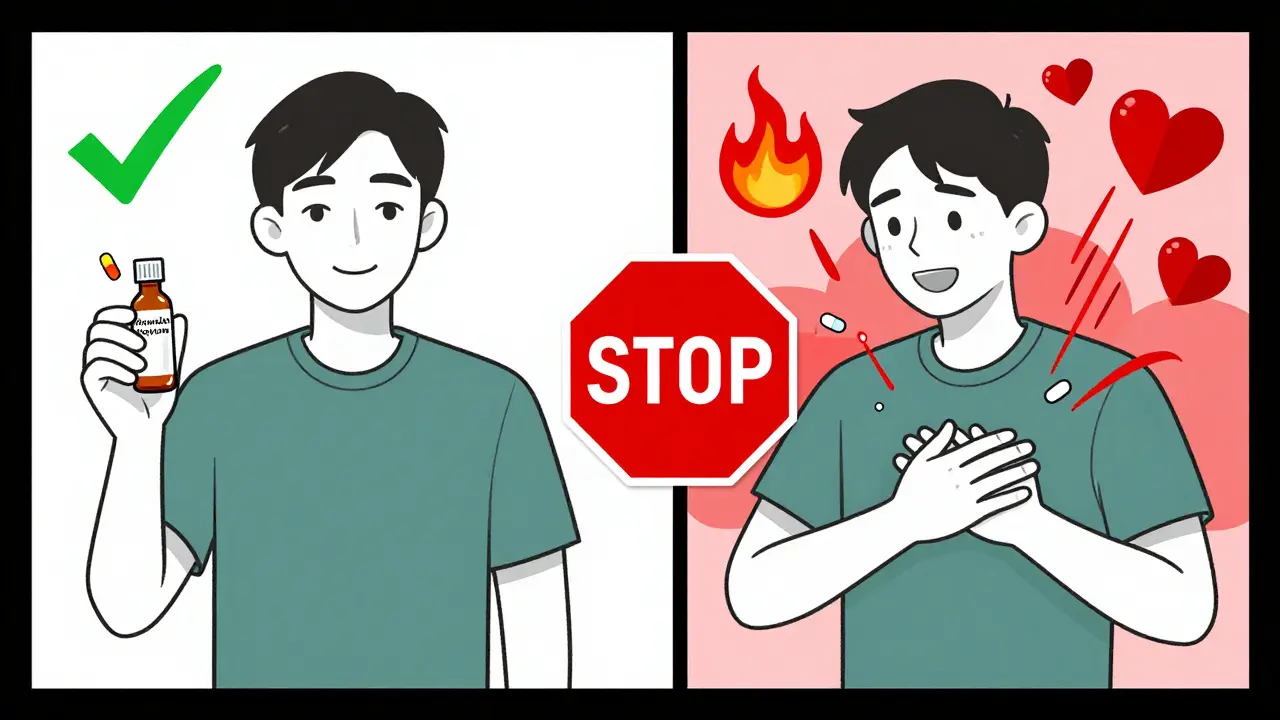
What Should You Do If You’re on Both?
Don’t panic. Most people take these drugs together without issue. But here’s how to stay safe:- Know your meds. Make a list of every drug you take, including over-the-counter ones like dextromethorphan or melatonin.
- Talk to your pharmacist. They check for interactions every time you fill a prescription. Ask: “Could this cause serotonin syndrome with my other meds?”
- Watch for symptoms. If you feel unusually restless, shaky, sweaty, or confused after starting a new drug, seek help immediately.
- Consider alternatives. For nausea, dexamethasone (a steroid) or metoclopramide (with caution) may be safer than ondansetron in high-risk patients.
- Ask about genetic testing. If you’re over 65 or on multiple serotonergic drugs, ask if CYP2D6 testing is right for you. It’s not routine-but it’s becoming more common.
In 2023, the American Geriatrics Society updated its Beers Criteria to specifically warn against using ondansetron in older adults on MAOIs and to use caution with SSRIs. That’s a clear signal: this isn’t theoretical. It’s in the guidelines.
What If It Happens?
If serotonin syndrome is suspected, stop all serotonergic drugs immediately. Don’t wait. Don’t “see how it goes.” Go to the ER. Treatment is straightforward:- Cyproheptadine (Periactin) is the first-line antidote. It blocks serotonin receptors. Dose: 4-8 mg orally, repeated every 2 hours until symptoms improve.
- Supportive care-cooling, IV fluids, oxygen, and monitoring.
- Dexmedetomidine is now being used in ICUs as an alternative to benzodiazepines. It reduces serotonin release by calming the nervous system.
Most people recover fully if treated early. But delays can lead to organ failure, seizures, or death. Time matters.
What’s Changing?
The field is evolving. Newer antiemetics like palonosetron (Aloxi) appear to carry less risk than ondansetron. A 2023 study showed switching from ondansetron to palonosetron reduced serotonin syndrome risk by over 60% in patients on SSRIs. That’s not because palonosetron is “safer”-it’s because it binds differently to serotonin receptors.Pharmaceutical companies are updating labels. GlaxoSmithKline added a “Serotonin Syndrome” warning to Zofran’s prescribing information in 2022 after 12 post-marketing cases. The FDA’s Sentinel Initiative reports a 29% increase in emergency visits involving antiemetics and serotonin syndrome between 2018 and 2022. The absolute numbers are still low-4.2 cases per 100,000 prescriptions-but the trend is upward.
What’s next? More personalized medicine. Genotyping for CYP2D6 status. Better decision tools for clinicians. But for now, awareness is your best defense.
Can ondansetron cause serotonin syndrome on its own?
No, ondansetron alone is extremely unlikely to cause serotonin syndrome. It’s designed to block serotonin receptors in the gut, not boost serotonin in the brain. Nearly all cases involve a combination with another serotonergic drug-like an SSRI, SNRI, or MAOI. The risk comes from the interaction, not the drug by itself.
Are all antiemetics risky for serotonin syndrome?
No. Only certain ones carry risk. 5-HT3 antagonists like ondansetron, granisetron, and dolasetron have a low but real risk when combined with other serotonergic drugs. Dopamine blockers like metoclopramide have moderate risk due to weak serotonin reuptake inhibition. NK1 antagonists like aprepitant pose minimal direct risk but can increase SSRI levels by slowing liver metabolism. Drugs like promethazine or prochlorperazine have very low serotonin activity and are safer choices in high-risk patients.
Is it safe to take ondansetron for morning sickness while on an SSRI?
It’s generally considered safe for short-term use, but caution is needed. The risk is low, but not zero-especially if you’re over 65, taking other serotonergic drugs, or are a poor CYP2D6 metabolizer. Many OB-GYNs prefer dexamethasone or doxylamine-pyridoxine for nausea in pregnancy because they have no serotonin activity. If ondansetron is used, stick to the lowest effective dose and avoid long-term use.
What are the early warning signs of serotonin syndrome?
Early signs include tremors, muscle stiffness, sweating, shivering, restlessness, rapid heartbeat, and mild confusion. These often appear within hours of taking a new drug or increasing a dose. If you’re on an SSRI and suddenly feel “electric” or jittery after getting ondansetron, don’t ignore it. These are red flags.
Should I stop my SSRI before getting ondansetron?
Never stop an SSRI without talking to your doctor. Abruptly stopping can cause withdrawal symptoms or make your mental health worse. Instead, inform your provider that you’re on an SSRI before getting any antiemetic. They can choose a safer alternative, adjust the dose, or monitor you more closely. The goal is to manage both conditions safely-not to sacrifice one for the other.


9 Comments
Oh please, like the FDA doesn’t know what’s going on. They’re paid off by Big Pharma to keep Zofran on the shelf while people die in ICU. You think they’d warn us if it was really dangerous? Nah. They’d rather keep selling $300 pills than admit their own drugs are killing people. This isn’t science-it’s corporate cover-up with a side of medical gaslighting.
I’m a nurse and I’ve seen this happen. A sweet 70-year-old woman got ondansetron after her hip surgery, was on sertraline, and within 2 hours she was trembling, sweating, and couldn’t tell her name from her cat’s. We had to stop everything, give cyproheptadine, and she was fine in 12 hours. Don’t panic-but please, please tell your doctor you’re on an SSRI before they give you that IV. It’s not hype, it’s real. 💔
Wait… so you’re telling me the government’s letting them give SSRIs to depressed people AND antiemetics to the same people… but they won’t tell us? 😳 This is definitely a mind control experiment. They want us docile, medicated, and confused so we don’t ask questions about the vaccines, the food, the 5G… this is just another layer. I knew it. I KNEW IT. 🤯
Let’s break this down. Ondansetron is a 5-HT3 antagonist-that means it blocks serotonin in the gut. But it has *weak* reuptake inhibition at 5-HT1A/2A receptors in the CNS. When combined with SSRIs-which block SERT-the net effect is increased synaptic serotonin. The risk is dose-dependent and metabolizer-dependent. CYP2D6 poor metabolizers? That’s a 2.3x spike in ondansetron exposure. That’s not theoretical-it’s pharmacokinetics 101. You don’t need conspiracy theories. You need to know your genotype. And if you’re over 65? Avoid it unless absolutely necessary. Simple.
i just wanted to say thank you for writing this. my mom is 71 and on fluoxetine and got ondansetron last year for nausea after chemo. she got really shaky and scared but the dr said it was just anxiety. i read this and cried because i knew something was off. i’m going to take her to a new dr next week and ask about dexamethasone. you’re helping people. ❤️
So let me get this straight-pharmacies are filling 22 million ondansetron scripts a year and nearly half of those go to people on SSRIs? And nobody’s auditing this? This isn’t negligence. This is genocide by prescription. They don’t care if you die as long as the insurance pays. Look at the FDA’s own data-29% increase in ER visits since 2018. That’s not a spike. That’s a slaughter. And the media won’t touch it because Big Pharma owns them. Wake up.
People think medicine is science but it’s just ritual. You swallow a pill because someone in a white coat told you to. You don’t ask why. You don’t question the system. You let them turn your body into a chemical cocktail and call it healing. Serotonin syndrome? That’s just the body screaming because you’ve forgotten how to be human. Stop outsourcing your health to corporations. Eat real food. Breathe. Walk in nature. That’s the real antidote.
Yeah right. Ondansetron is dangerous? Tell that to the 99.9% of people who take it and don’t turn into a human vibrator. This article is fearmongering dressed up as science. If you’re on an SSRI and get nauseous, take a nap. Drink ginger tea. Don’t let some overworked ER doc scare you into avoiding a drug that saved your life after chemo. Stop looking for dangers in every pill. The world’s not out to get you. It’s just… boring.
This is a well-researched and balanced overview. Thank you for highlighting both the risks and the context. While the absolute risk is low, the potential consequences are severe enough that awareness should be standard-not optional. In my practice in India, we rarely see this due to lower SSRI use and different prescribing patterns, but the principles apply universally. A simple conversation between patient and provider can prevent tragedy. Knowledge is the most accessible medicine we have.