More than 1 in 10 people in the U.S. think they’re allergic to a drug. But here’s the problem: most of them aren’t. A lot of people mistake side effects - like a stomachache from antibiotics or a headache from blood pressure meds - for true allergies. That’s dangerous. If you’re wrongly labeled as allergic to penicillin, your doctor might give you a stronger, pricier, riskier antibiotic instead. And that can lead to longer illnesses, hospital stays, or even deadly infections like C. diff.
So how do you tell the difference between a side effect and a real drug allergy? And when should you rush to the ER? This isn’t about guessing. It’s about recognizing patterns - the kind doctors use to make life-or-death calls.
What a Real Drug Allergy Actually Looks Like
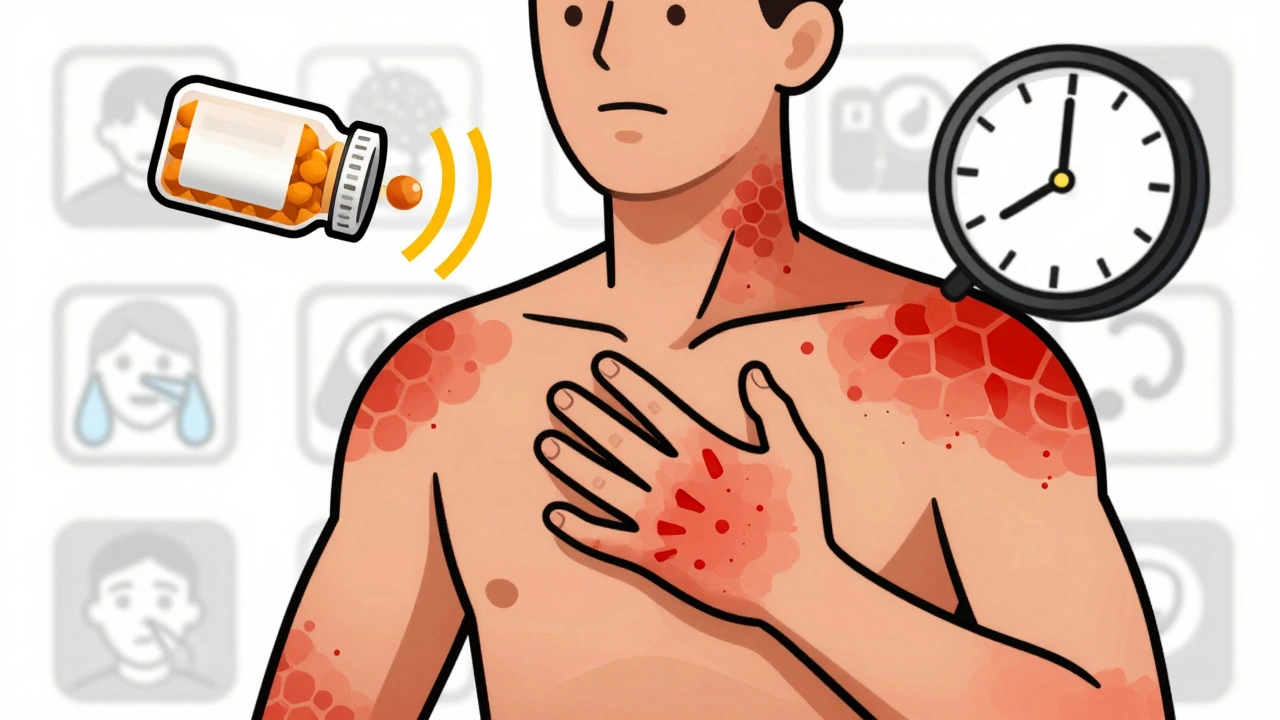
A true drug allergy means your immune system thinks the medicine is an invader. It’s not just feeling sick. It’s your body launching a targeted attack. That’s why reactions vary so much - your immune system can target your skin, lungs, gut, or even your blood pressure.
The most common sign? A rash. But not just any rash. A drug rash often shows up as red, raised bumps (hives) that itch badly. They might spread fast. Or they could be flat, red spots that look like measles. These usually show up days after you start the drug - sometimes even weeks later.
But here’s what you can’t ignore: if you have a rash AND trouble breathing, swelling in your throat, or dizziness - call 911 right now. That’s not a rash. That’s anaphylaxis. It’s a full-body reaction that can kill you in minutes.
Timing Matters: When Symptoms Show Up Tells You a Lot
Not all drug reactions happen the same way. The clock starts ticking the moment you take the pill.
- Within minutes to an hour: This is the red zone. Think hives, swelling of the lips or tongue, wheezing, vomiting, or passing out. These are signs of IgE-mediated reactions - the kind that lead to anaphylaxis. Penicillin, sulfa drugs, and some painkillers like ibuprofen or naproxen are common triggers.
- Days later: A flat, itchy rash that spreads slowly? That’s a delayed exanthem. It’s common with antibiotics like amoxicillin. You might feel fine otherwise - no fever, no swelling. Still, stop the drug and call your doctor.
- One to three weeks later: Fever, swollen lymph nodes, joint pain, and a rash? That could be serum sickness-like reaction. It’s rare but serious. Sometimes it’s triggered by antibiotics or biologics.
- Two to six weeks later: A blistering rash that peels off like a burn, with sores in your mouth or eyes? That’s Stevens-Johnson Syndrome or Toxic Epidermal Necrolysis. It’s life-threatening. You need emergency care immediately.
Some reactions are even sneakier. DRESS syndrome - Drug Rash with Eosinophilia and Systemic Symptoms - can start like a mild rash, then turn into liver failure or kidney damage weeks later. You might feel fine at first. That’s why it’s so easy to miss.
What to Do If You Think It’s an Allergy
If you notice any of these symptoms after taking a new drug, stop taking it. Don’t wait. Don’t hope it goes away.
Call 911 or go to the ER if you have:
- Difficulty breathing or wheezing
- Swelling of the face, lips, tongue, or throat
- Feeling faint, dizzy, or passing out
- Fast heartbeat or low blood pressure
- A rash with blistering or peeling skin
- High fever with rash and swollen glands
These aren’t signs to "wait and see." They’re emergency signals. Anaphylaxis doesn’t wait. Neither should you.
If it’s a mild rash with no other symptoms - no trouble breathing, no swelling - you still need to act. Take a photo of the rash. Write down the name of the drug, when you took it, and when the rash started. Call your doctor. Don’t just say, "I think I’m allergic." Say, "I took amoxicillin on Tuesday. On Thursday, I got this rash. Here’s a photo." Details matter.

Why Misdiagnosing a Drug Allergy Is a Big Deal
Let’s say you think you’re allergic to penicillin. You’ve had a rash once, years ago. So you tell every doctor. They avoid penicillin. They give you something else - maybe vancomycin or ciprofloxacin. Those drugs are broader. They kill more bacteria. But they also kill good bacteria. That’s why people with false penicillin allergies are 50% more likely to get a C. diff infection - a nasty, hard-to-treat gut infection that causes severe diarrhea and can be deadly.
And here’s the kicker: over 90% of people who think they’re allergic to penicillin aren’t. When they get tested properly, they can take it safely. But because no one ever tested them, they’ve spent decades avoiding the safest, cheapest, most effective antibiotic on the planet.
Mislabeling doesn’t just hurt you. It hurts the whole system. More expensive drugs. Longer hospital stays. More antibiotic resistance. It’s a public health problem hiding in plain sight.
How Doctors Confirm a Drug Allergy
There’s no blood test for most drug allergies. No quick lab result. The best tool? Your story - and a trained allergist.
For penicillin, there’s a gold standard: skin testing. A tiny drop of penicillin is placed on your skin, then gently pricked. If you’re allergic, a red, itchy bump shows up within 15 minutes. If that’s negative, they might give you a small oral dose under supervision. If you stay fine? You’re not allergic.
For other drugs? It’s harder. For reactions like DRESS or SJS, doctors might check blood for high white cell counts or liver enzymes. But even then, it’s not foolproof. That’s why specialists are critical. General doctors don’t get trained to spot these patterns. Allergists do.
If you’ve had a serious reaction - especially one that involved breathing, swelling, or skin peeling - you need to see an allergist. Not your GP. Not the urgent care center. An allergist who specializes in drug hypersensitivity. They’ll map out your history, run the right tests, and give you a clear answer: "You’re allergic," or "You’re not."

What to Do After You Know You’re Allergic
Once you’re confirmed as allergic to a drug, you need to protect yourself. Here’s how:
- Get a medical alert bracelet. It should say exactly what you’re allergic to - not just "drug allergy." Say "Penicillin Allergy" or "Sulfa Allergy."
- Keep a written list. Put it in your phone, wallet, and email. Include the drug name, the reaction you had, and the date.
- Tell every doctor, dentist, and pharmacist. Even if they don’t ask. Say it loud: "I’m allergic to [drug]. I had [symptom]."
- Ask about alternatives. If you’re allergic to one NSAID, you might still be fine with another. Don’t assume they’re all the same.
- Don’t assume cross-reactivity. Being allergic to penicillin doesn’t mean you’re allergic to all antibiotics. Only some share similar structures. Your allergist can tell you which ones are safe.
And if you’re ever in doubt - if you’re taking a new drug and feel something strange - stop it. Call your doctor. Take a photo. Don’t risk it.
Final Thought: Don’t Guess. Get Tested.
Drug allergies aren’t something you should live with based on a memory from 10 years ago. They’re not a label you should accept without proof. They’re a medical condition - and like any condition, they need accurate diagnosis.
If you’ve ever had a reaction to a drug - even a mild one - ask yourself: Did I get tested? Did I see a specialist? Or did I just assume I’m allergic because I felt a little sick?
Getting it right isn’t just about avoiding a rash. It’s about avoiding the wrong antibiotic. It’s about avoiding a hospital stay. It’s about living without unnecessary risk.
One phone call to an allergist could change the way you’re treated for the rest of your life.
How do I know if my rash is from a drug allergy or just a side effect?
A side effect is usually predictable and tied to how the drug works - like nausea from antibiotics or dizziness from blood pressure meds. A true drug allergy involves your immune system and often includes itching, hives, swelling, or trouble breathing. If you have a rash plus any of those symptoms, it’s likely an allergy. If it’s just a rash with no other symptoms, it could still be an allergy - but it’s harder to tell. Always get it checked by a doctor.
Can I outgrow a drug allergy?
Yes, especially with penicillin. Many people lose their sensitivity over time. Studies show that 80% of people who were allergic to penicillin 10 years ago can now take it safely. That’s why retesting is so important. Don’t assume you’re still allergic just because you had a reaction in the past.
Is there a blood test for drug allergies?
For most drugs, no. Blood tests aren’t reliable for diagnosing common allergies like penicillin or sulfa. The only exception is for severe delayed reactions like DRESS syndrome, where doctors might check for high eosinophils or liver enzymes. Skin testing and oral challenges are still the gold standard - but only for a few drugs. For others, your history and symptoms are the main tools.
What if I have a reaction but don’t know what caused it?
Write down everything: all the medications you took in the last 7 days, supplements, even over-the-counter pills. Take photos of any rash or swelling. Then see an allergist. They’ll help you narrow it down. Don’t wait. Even if the reaction was mild, knowing the cause helps prevent a worse one next time.
Can I take a different drug in the same class if I’m allergic to one?
Sometimes. For example, if you’re allergic to amoxicillin (a penicillin), you might still be able to take a cephalosporin - but not always. Cross-reactivity isn’t guaranteed. Only an allergist can test this safely. Never assume two drugs are safe just because they’re "similar." Always get tested before trying another.
What should I do if I’m allergic to a drug but need it for a serious condition?
If the drug is essential - like penicillin for a life-threatening infection - your allergist may do a desensitization procedure. This involves giving tiny, increasing doses under close supervision. It’s not for everyone, but it can be lifesaving when no other options exist. Never try this at home. It must be done in a hospital or allergy clinic.
Next Steps: Protect Yourself Before It’s Too Late
If you’ve ever had a reaction to a drug - even if it was "just a rash" - schedule a visit with an allergist. Bring your photos, your notes, your list of medications. Don’t wait until you’re in the ER.
If you’ve been told you’re allergic to penicillin, get tested. It’s safe. It’s quick. And it could change your entire medical future.
And if you’re ever in doubt - if you feel something strange after taking a new pill - stop it. Call your doctor. Take a picture. Don’t guess. Get it checked.


12 Comments
OMG I thought I was allergic to penicillin for 15 years 😭 Turned out it was just a stomachache from the antibiotics. Got tested last year and now I can take it safely-saved me $2k in co-pays and a 3-day hospital stay. You guys NEED to get checked if you think you’re allergic.
It’s not just about penicillin… it’s about the entire medical-industrial complex weaponizing misdiagnosis to push expensive, patent-protected antibiotics… the CDC knows this… they’ve published papers… but no one wants to admit that profit drives overprescription… and we’re the guinea pigs…
And don’t even get me started on how pharma companies lobby to avoid liability for adverse reactions… it’s systemic… it’s predatory… it’s capitalism…
They’re lying. The FDA knows 90% of these ‘allergies’ are fake because they don’t want to admit how many people they’ve poisoned with broad-spectrum antibiotics. You think this is about safety? No. It’s about controlling the narrative. The CDC, AMA, Big Pharma-they all collude. I’ve seen the emails. They call it ‘antibiotic stewardship’-but it’s just cover for killing off the cheap meds so they can sell you the expensive ones.
And if you’re lucky enough to get skin-tested? They’ll still charge you $800. Then they’ll say ‘you’re fine’-but you’ll never trust them again. I’m not taking anything until I see the lab results myself. And I’ve got 3 lawyers on retainer.
As a pharmacist in Mumbai, I see this EVERY DAY. People self-diagnose allergies because they got a rash after one pill and now they avoid ALL antibiotics. Then they come back with C. diff or sepsis. We need more public awareness-especially in developing countries where alternatives are scarce. Please, if you have a rash, don’t panic-just call your doctor. And if you’re in the US, go see an allergist. It’s life-changing.
I appreciate how clearly this breaks down the difference between side effects and true allergies. I used to think any rash meant I was allergic-until I had a mild reaction to amoxicillin and then spent six months with a specialist who did skin testing and an oral challenge. Turns out, I’m not allergic at all. Now I take penicillin without fear, and I’ve saved my insurance thousands. I wish I’d done this ten years ago. If you’ve ever had a reaction-even a small one-please, please, please don’t assume. Get tested. It’s not complicated, it’s not scary, and it could literally save your life.
Just got my penicillin skin test done last week-negative!! 🎉 I’ve been avoiding it since I was 12. Now I can take the cheap stuff and not worry about C. diff. Thank you for this post!!
While the intent of this article is commendable, the lack of rigorous citation to peer-reviewed studies-particularly regarding the 90% false-positive rate-is problematic. Furthermore, the conflation of IgE-mediated reactions with delayed hypersensitivity is a gross oversimplification. One must consider the pharmacokinetics of beta-lactams, the role of HLA haplotypes in SJS/TEN, and the absence of validated biomarkers for non-IgE reactions. This is not a public service announcement-it’s a poorly sourced blog post masquerading as medical advice.
I’m a nurse who’s seen this happen too many times. A patient comes in with a rash after amoxicillin, says they’re allergic, and we give them vancomycin. Three days later, they have C. diff and are in septic shock. I’ve had families cry because they didn’t know their ‘allergy’ was a lie. Please, if you think you’re allergic-get tested. Don’t let fear make you sicker. And if you’ve been told you’re allergic, ask your doctor: ‘Can I be tested?’ It’s not rude. It’s smart.
My sister had a rash after penicillin. Went to ER. They said ‘allergy.’ She avoided all antibiotics for 8 years. Got pneumonia last year. Had to be intubated. Turned out she wasn’t allergic. They did a skin test. Negative. She’s fine now. But she almost died because no one ever questioned the label. 🤦♀️
Don’t assume. Get tested. It’s 15 minutes. Worth it.
i had a rash after amoxicillin when i was 5 and never took it again. now im 34 and just got tested and turns out im not allergic?? like… i’ve been avoiding the best antibiotic for 29 years?? wow. thanks for the post!!
What’s next? Are we going to start questioning if people are really allergic to peanuts? Or gluten? Or vaccines? This is how the anti-vaxxers start. You can’t just ‘test’ your way out of being allergic. If your body reacted once, it’s still allergic. You’re just being manipulated by Big Pharma to buy more drugs. Trust your body, not the system.
Thank you for this clear and necessary explanation. In India, many patients are labeled as allergic to antibiotics based on childhood rashes, leading to inappropriate treatment and rising resistance. I have shared this with my community clinic. Every doctor should read this. A simple skin test can prevent years of unnecessary risk. Please, if you have a history-get evaluated. Not assumed. Tested.