Diabetic retinopathy isn’t just a complication of diabetes-it’s the leading cause of preventable vision loss in adults under 65. And here’s the hard truth: diabetic retinopathy often has no symptoms until it’s advanced. By the time blurry vision or dark spots show up, damage may already be irreversible. But the good news? With the right screening and timely treatment, up to 98% of severe vision loss from this condition can be prevented.
How Often Should You Get Screened?
The old rule-get an eye exam every year-isn’t right for everyone anymore. Thanks to decades of research, we now know that screening frequency should match your personal risk, not just your diabetes diagnosis. The key is knowing your level of retinopathy and what’s driving its progression.If you have no signs of retinopathy and your blood sugar (HbA1c) is under 7%, blood pressure is controlled, and your kidneys are healthy, you can safely stretch your screening to every 2-3 years. Studies show that patients with two clean screenings in a row have almost zero risk of developing sight-threatening damage in that time. The UK’s National Screening Committee updated its guidelines in 2016 based on this data, and it’s now standard practice in many countries.
But if you have even mild nonproliferative diabetic retinopathy (NPDR), you need to step up your game. That means seeing an eye specialist every 6-12 months. If you’re at the moderate NPDR stage, you should be referred to an ophthalmologist within 3-6 months. Severe NPDR? That’s a red flag-you need to be seen within 3 months. And if you’ve reached proliferative diabetic retinopathy (PDR), you’re at immediate risk of bleeding or retinal detachment. You need to be evaluated within 30 days.
There’s a tool called RetinaRisk that’s changing how doctors decide your schedule. It uses your HbA1c, diabetes duration, blood pressure, and kidney function to calculate your risk score. For someone with low risk, it might suggest screening every 5 years. For someone with high risk-say, HbA1c over 9%, long-standing diabetes, and early kidney damage-it might say every 6 months. This personalized approach cuts unnecessary visits by nearly 60% without missing a single case of sight-threatening disease.
What About Type 1 vs. Type 2 Diabetes?
People with type 1 diabetes usually start screening 3-5 years after diagnosis, because retinopathy rarely shows up before then. But for type 2, screening should begin right at diagnosis. Why? Because many people have had undiagnosed high blood sugar for years before their type 2 diagnosis. By the time they’re diagnosed, retinopathy may already be present.Even if you’ve had type 1 diabetes for 20 years, if your HbA1c has stayed under 7% and you’ve had no signs of retinopathy in your last two screenings, you can go 2-3 years between exams. The DCCT/EDIC study, which followed over 1,400 people for decades, proved that tight control doesn’t just slow progression-it can actually reverse early damage. But if your HbA1c has been above 8% for the last year, or your blood pressure is consistently over 140/90, annual screening is still the safest bet.
And don’t forget pregnancy. If you’re diabetic and pregnant, your risk of retinopathy worsening skyrockets. Screenings should happen in the first trimester and then every 3 months until delivery. Hormonal changes and rapid blood sugar shifts can accelerate damage in weeks, not years.
How Is Diabetic Retinopathy Detected?
Screening isn’t just a quick glance with a light. It’s a detailed retinal photo session. The gold standard is mydriatic digital fundus photography-your pupils are dilated, and high-resolution images are taken of the back of both eyes. Two standard views are captured: one centered on the macula (the center of vision) and one on the optic nerve. These images are graded using the International Clinical Diabetic Retinopathy Scale, which has five levels: no retinopathy, mild NPDR, moderate NPDR, severe NPDR, and proliferative DR.Diabetic macular edema (DME) is a separate but common problem. It’s fluid buildup in the macula that causes swelling and blurring. It can happen at any stage of retinopathy, even with mild NPDR. That’s why images must include the macula. If DME is suspected, you’ll need an OCT scan (optical coherence tomography), which gives a 3D cross-section of the retina.
AI is now playing a big role. Algorithms like Google’s DeepMind and IDx-DR can analyze retinal photos with over 94% accuracy in spotting referable disease. In rural areas where ophthalmologists are scarce, telemedicine platforms let primary care nurses take photos and send them to specialists for remote review. One study in the U.S. found that tele-screening caught 94% of cases that an eye doctor would have flagged.

What Are the Treatment Options?
Treatment depends on how far the disease has gone. For early stages-mild to moderate NPDR-the best treatment is still tight control of blood sugar, blood pressure, and cholesterol. No eye drops. No laser. Just better management. The DCCT study showed that intensive control reduced the risk of retinopathy by 76% in type 1 diabetes.When you reach severe NPDR or PDR, laser treatment (panretinal photocoagulation) is often the first step. It doesn’t restore vision, but it shrinks abnormal blood vessels that can bleed or tear the retina. It’s done in one or two sessions, takes less than an hour, and is usually painless after numbing drops.
For diabetic macular edema, injections are the go-to. Anti-VEGF drugs like ranibizumab (Lucentis), aflibercept (Eylea), and bevacizumab (Avastin) block the growth of leaky blood vessels. You’ll get shots in the eye every 4-8 weeks at first, then less often as the swelling improves. Studies show these injections can improve vision in 40-50% of patients and stop vision loss in over 90%.
In advanced cases, vitrectomy surgery may be needed. This removes blood or scar tissue from inside the eye. It’s more invasive, but for people with massive bleeding or tractional retinal detachment, it’s often the only way to save sight.
And here’s something new: newer drugs like faricimab (Vabysmo) are now approved for both DME and PDR. They work longer between doses-some patients can go 3-4 months between injections instead of monthly. That’s a big win for quality of life.
Why Do So Many People Miss Their Screenings?
Even though screening saves sight, only about 60% of people with diabetes in the U.S. get their recommended eye exams each year. In Australia, it’s a bit better-around 70%-but still far from ideal.Barriers are real. Some people don’t feel sick, so they skip it. Others can’t get an appointment. Rural areas often lack access to imaging equipment. Insurance doesn’t always cover it. And confusion about changing guidelines doesn’t help. One Reddit user wrote: ‘My clinic pushed for 2-year intervals despite my HbA1c being 8.5%. I developed macular edema that could’ve been caught earlier.’
On the flip side, many patients report relief when their intervals are extended. ‘After three clean screenings, my doctor switched me to every two years,’ said another user. ‘I used to dread the appointments. Now I actually feel more in control.’
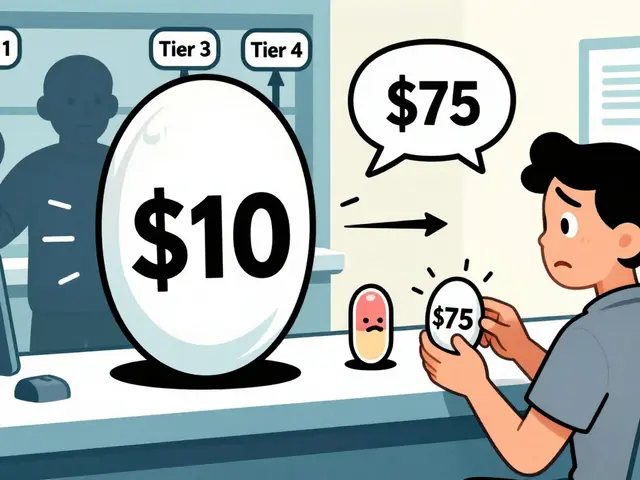
Cost is another factor. In the U.S., a screening can cost $45-$65 under Medicare. In the UK, it’s free through the NHS. But in places without universal care, even $50 can be a barrier. That’s why telehealth and smartphone-based tools like the D-Eye adapter (FDA-cleared in 2021) are growing fast. They let your primary care provider take the photo right in the office.

What’s Changing in 2025?
The biggest shift is moving from a one-size-fits-all approach to true personalization. The American Diabetes Association’s 2024 Standards now say: ‘If you’ve had no retinopathy and your HbA1c is in target, screening every 1-2 years may be considered.’ That’s a huge change from the old ‘annual for everyone’ rule.AI tools are getting smarter and cheaper. Some systems now predict not just current disease, but future risk-like whether you’re likely to develop DME in the next 12 months. That means screenings can be timed even more precisely.
Global efforts are scaling up. The World Health Organization estimates that if risk-stratified screening is rolled out worldwide, we could prevent 2.5 million cases of blindness by 2030. That’s a 40% drop in diabetes-related vision loss.
But equity remains a problem. Low-income communities and minority groups have the same rate of diabetes, but 2.3 times higher rates of vision loss. Why? Less access to screening, less consistent care, and later diagnosis. Fixing this isn’t just a medical challenge-it’s a social one.
What Should You Do Right Now?
If you have diabetes, here’s your action plan:- Get your first retinal screening as soon as possible-right after diagnosis for type 2, or 3-5 years after diagnosis for type 1.
- Know your HbA1c, blood pressure, and kidney function numbers. These determine your risk level.
- Ask your doctor: ‘Based on my numbers, how often should I be screened?’ Don’t accept ‘every year’ without context.
- If you’re told you have no retinopathy, ask if you qualify for extended intervals (every 2-3 years).
- If you’re told you have mild or worse retinopathy, get a referral to an ophthalmologist immediately.
- Keep your HbA1c under 7%, blood pressure under 140/90, and avoid smoking. These are your best defenses.
Diabetic retinopathy doesn’t have to steal your sight. But it won’t stop unless you act. The tools, the science, and the guidelines are here. Now it’s about using them.
Can diabetic retinopathy be reversed?
Early stages of diabetic retinopathy, especially mild nonproliferative retinopathy, can improve with strict blood sugar and blood pressure control. The DCCT/EDIC study showed that people who maintained HbA1c below 7% saw regression of early retinal changes over time. But once damage reaches the proliferative stage or causes macular edema, the goal shifts from reversal to stopping further damage. Treatments like laser and injections can stabilize vision, but they rarely restore lost sight.
Is diabetic retinopathy screening covered by insurance?
In the U.S., Medicare and most private insurers cover annual diabetic eye exams as a preventive service under the Diabetes Prevention and Control Act. In Australia, Medicare covers retinal photography under the Medicare Benefits Schedule (item number 15400) for eligible patients. In the UK, the NHS provides free annual screening through its national program. Always confirm with your provider, but in most cases, if you have diabetes, this screening is included.
Do I need to get my pupils dilated every time?
For the most accurate screening, yes-dilation gives a wider, clearer view of the retina. However, some newer non-mydriatic cameras can capture good images without dilation, especially in low-risk patients. But if your doctor suspects any signs of disease or you’re being monitored for progression, dilation is still the standard. The benefits of catching early damage outweigh the temporary discomfort of blurred vision for a few hours.
Can I rely on my vision to tell me if I have diabetic retinopathy?
No. Diabetic retinopathy often progresses without any symptoms until it’s advanced. Many people have moderate to severe retinopathy and still see clearly. That’s why screening is critical-even if your vision feels fine. By the time you notice blurriness, floaters, or dark spots, the damage may already be permanent. Don’t wait for symptoms to act.
How long do eye injections for diabetic macular edema last?
Traditional anti-VEGF injections like Lucentis or Eylea typically require monthly shots at first, then every 6-8 weeks as the condition stabilizes. Newer drugs like Vabysmo can last up to 4 months between doses for some patients. The duration depends on your body’s response, how much swelling was present at the start, and whether your blood sugar and blood pressure are well-controlled. Most patients need ongoing treatment-this isn’t a one-time fix.
Are there any natural remedies or supplements that help?
No supplement has been proven to treat or prevent diabetic retinopathy. Some studies looked at antioxidants, omega-3s, or bilberry, but none showed consistent clinical benefit. The only proven interventions are controlling blood sugar, blood pressure, and cholesterol, plus medical treatments like laser and injections. Be wary of products claiming to ‘cure’ retinopathy-they’re not backed by science and can delay real care.
What happens if I skip my screening for a year?
If you’re low-risk-with no retinopathy, HbA1c under 7%, and healthy kidneys-skipping a year is unlikely to cause harm. But if you have any signs of retinopathy, or your HbA1c is above 8%, skipping even one year can mean missing the window to prevent vision loss. Rapid progression can happen in people with uncontrolled diabetes, especially during pregnancy or illness. When in doubt, follow your doctor’s personalized schedule.


15 Comments
Just got my annual eye check and they said I can go 3 years now because my HbA1c is 6.8 and BP’s stable. Feels weird to not be chased by appointments every year-but also kinda empowering? Like, my body’s listening.
Still terrified of the next one though. 😅
Let me tell you, I used to think diabetic retinopathy was just one of those scary things doctors threw out to scare you into taking your meds-until I saw the actual images from my fundus photo. There were tiny hemorrhages, like little red stars on the back of my eye. I didn’t feel a thing. Zero symptoms. And that’s the scariest part. This isn’t a ‘maybe’-it’s a silent thief. The fact that we can now predict risk with tools like RetinaRisk? That’s not just science-that’s a lifeline. I used to skip screenings because I felt fine. Now I schedule them like dentist appointments. Because vision isn’t something you get back.
Also, if you’re thinking ‘I’ll just wait till I see blurriness’-stop. Right now. Go call your doctor. Your future self will thank you.
The shift toward risk-stratified screening represents a significant evolution in clinical guidelines, grounded in longitudinal data from the DCCT/EDIC cohort and supported by recent meta-analyses published in JAMA Ophthalmology. The reduction in unnecessary visits-nearly 60%-without compromising detection rates is a compelling argument for personalized medicine in chronic disease management. That said, equitable access remains a critical concern, particularly in underserved communities where telehealth infrastructure is underdeveloped. The WHO’s projection of 2.5 million prevented blindness by 2030 is ambitious but achievable, contingent upon systemic investment in screening logistics and provider training.
It is imperative that policy makers recognize this not merely as a medical intervention, but as a public health imperative.
I used to cry after every eye appointment. Not because it hurt-but because I felt like I was failing. My HbA1c was always hovering around 8.5. I’d look at the photos and think, ‘That’s my fault.’ Then I found a diabetic educator who didn’t judge me. She said, ‘Your body is still fighting. That’s not failure. That’s resilience.’
So I stopped obsessing over numbers and started obsessing over habits. Walking after dinner. Sleeping seven hours. Not skipping meals. And guess what? My last screening showed regression in the microaneurysms. Not cured. Not perfect. But better.
Diabetes doesn’t own me. I’m not a statistic. I’m a person trying. And that’s enough.
Also-Vabysmo? I got my first shot last month. Four months between injections? I almost cried again. This time from relief.
Man, I used to think eye doctors were just glorified photographers with fancy lenses. Then I watched my uncle lose half his vision because he skipped his screenings for three years ‘because he felt fine.’ Now I’m the guy who shows up with a printout of his HbA1c, BP, and kidney numbers and says, ‘So… what’s my RetinaRisk score?’
And let me tell you-the AI tools? They’re not magic. But they’re honest. No fluff. No ‘come back next year’ unless you’ve earned it. I’ve got a cousin in Texas who’s got type 2 and works two jobs. She got her retinal scan done at her primary care doc’s office with a handheld camera. No dilation. No waiting. $35 out of pocket. That’s the future. Not some fancy clinic in the city. Right here. Right now.
Stop waiting for the perfect moment. The perfect moment is when you’re still able to see your kid’s face.
Wait-so if I’ve had two clean screenings and my HbA1c is under 7%, I can go 3 years?! That’s insane. My doctor still makes me come every year like I’m on probation. And I’ve been under 6.5 for two years straight! What’s the point of all this ‘personalized’ nonsense if they’re still treating everyone like they’re a ticking time bomb?
Also-why is Avastin cheaper than Eylea? Is it just because it’s not branded? Should I ask for the ‘cheap one’? Is it safe? Do I have to Google this every time? Someone please tell me I’m not the only one who feels like a lab rat in a diabetes circus.
And also-can we PLEASE stop calling it ‘diabetic retinopathy’ like it’s a personality trait? It’s a complication. Not my identity.
They say AI detects retinopathy with 94% accuracy but the FDA approved it and the CDC says its fine so its fine right? I mean why would they lie about this? Theyre all in the pocket of Big Pharma anyway. You think they really want you to see better? Nah. They want you coming back every month for shots. That’s where the money is. You think they’d let you go 4 months between injections if it wasn’t profitable? Think again. And why is it free in the UK but not here? Coincidence? I think not. They’re controlling you with fear. Skip the screening. Eat less sugar. That’s all you need. I’ve been diabetic 15 years and my eyes are fine. No shots. No lasers. Just willpower.
Also-dilation? That’s a scam. They just want you to be blind for a few hours so you’ll buy more meds.
Wow. Someone actually wrote a 2000-word essay on eye exams. How touching. Let me guess-you got your HbA1c down to 6.2 and now you’re the pope of diabetic retinopathy? Congrats. You’re not special. You’re just lucky.
Meanwhile, my cousin’s mom went blind because she trusted ‘extended intervals’ and skipped her checkup for 18 months. Turns out ‘low risk’ doesn’t mean ‘immune.’
And you’re telling people to ‘ask their doctor’? Good luck with that. Most docs don’t even know what RetinaRisk is. They just copy-paste the same script from the pamphlet.
Don’t believe the hype. The system doesn’t care if you see. It just cares if you pay.
I’m a nurse who works with diabetic patients every day. I’ve seen people cry because they were told they needed injections. I’ve seen others refuse to believe they had retinopathy because ‘they could still read the clock.’
But here’s what I’ve learned: the people who survive this without losing vision? They’re not the ones with the best numbers. They’re the ones who showed up. Even when they were scared. Even when they were tired. Even when they felt guilty.
You don’t have to be perfect. You just have to be present.
And if your doctor won’t give you a personalized plan? Find another one. Your sight is worth it.
Just had my first Vabysmo shot. Four months between injections? I’m already planning my vacation. No more monthly eye clinic trips. No more ‘don’t drive for 2 hours’ warnings. I feel like I got my life back.
And yeah, I still have diabetes. But I don’t have to live in fear anymore. This isn’t just medicine-it’s freedom.
If you’re scared of injections? I was too. But it’s less scary than losing your sight. And honestly? The numbing drops make it feel like a tiny pinch. Like a mosquito that gives you a hug.
Don’t wait. Go get checked. Your future self is already thanking you.
The clinical evidence supporting risk-stratified screening intervals is robust, particularly when validated against longitudinal datasets such as the UKPDS and DCCT/EDIC. However, the implementation of AI-driven tools like IDx-DR requires rigorous validation in diverse populations, as algorithmic bias may arise from training datasets lacking ethnic and socioeconomic diversity. Furthermore, the economic burden on non-Universal Healthcare systems remains a significant barrier to equitable access, particularly for migrant populations and undocumented individuals. While technological innovation is commendable, systemic reform is non-negotiable.
My dad lost his vision in his 50s because he thought ‘I don’t feel sick, so I’m fine.’ He didn’t go for 4 years. One day he couldn’t see his grandkids’ faces. He cried for three days.
Now I go every year. Even when I’m tired. Even when I’m broke. Even when I don’t want to.
Because I don’t want to be the reason my kid grows up without seeing me smile.
It’s not about the HbA1c. It’s about showing up.
And if you’re reading this and you’ve skipped a screening? Just go. Please. For them.
The integration of AI into retinal screening represents a paradigm shift in preventive ophthalmology. The key advantage lies in scalability: a single trained technician can capture images for 50 patients in a day, with remote grading by a single ophthalmologist. This model has proven effective in rural India and Appalachia, where specialist access is limited. However, human oversight remains essential-AI can detect lesions, but not context. A patient’s social history, adherence patterns, and psychosocial stressors influence progression in ways algorithms cannot yet quantify. The future of screening is hybrid: AI for efficiency, clinicians for nuance.
And yes-it works. I’ve seen it.
They say ‘98% of vision loss is preventable’-but who’s paying for all these scans? The government? The hospitals? The taxpayers? Meanwhile, we’re getting deported for not having insurance, but somehow we’re supposed to get free eye checks? This is socialism with a retina filter. You want to save sight? Stop giving free stuff to people who won’t take care of themselves. Let them pay. Let them suffer. Then maybe they’ll learn.
And why is this even a thing? Diabetes is a lifestyle disease. If you’re eating pizza and soda, don’t blame the eye doctor. Blame yourself.
I had retinopathy and I didn’t even know it! I cried for three days when I found out! Everyone around me was so mean! They said ‘you should’ve gone sooner’ but no one helped me! I’m just a girl trying to survive! My husband doesn’t understand! My boss thinks I’m lazy because I take time off for eye appointments! I’m not like other people! I have trauma! I’m not just a number on a chart! I’m a soul! And now I have to get injections every month and I’m scared to death! WHO WILL HOLD MY HAND?!
And why is this so expensive?! Why can’t they just fix it with a miracle? Why does everything have to hurt?! I just want to see my cat again without squinting!!