
For decades, women have been told to use backup contraception when taking antibiotics. You get a prescription for amoxicillin for a sinus infection, and the pharmacist hands you a packet of condoms with a warning: "Better safe than sorry." But what if that warning is based on a myth? The truth is, antibiotics and birth control pills don’t usually interfere - except for one very specific group.
The Myth That Won’t Die
It started with a few scattered case reports in the 1970s. A woman on birth control got pregnant while taking an antibiotic. The assumption? The antibiotic ruined her pill. That idea stuck. Even today, nearly two out of three women believe antibiotics reduce birth control effectiveness. A 2022 Planned Parenthood survey found that 62% of patients thought this was true. Pharmacies still hand out condoms as a default. Social media groups like "Birth Control Support" get hundreds of anxious posts every month asking the same question: "Can antibiotics make me pregnant?" But here’s the problem: most of those early cases weren’t about regular antibiotics. They were about rifampin - a drug used to treat tuberculosis. And that’s the only antibiotic class with solid, proven evidence of messing with hormonal birth control.Only One Type of Antibiotic Actually Interferes
The Centers for Disease Control and Prevention (CDC) and the American College of Obstetricians and Gynecologists (ACOG) both say the same thing: for most antibiotics, there’s no risk. That includes the ones you get most often - amoxicillin, azithromycin, doxycycline, metronidazole, ciprofloxacin, and even clarithromycin. These drugs don’t lower hormone levels enough to affect birth control. A 2011 review of 14 studies confirmed that penicillin-type antibiotics don’t change estrogen absorption. A 2020 CDC analysis of 35 clinical trials showed that non-rifamycin antibiotics kept hormone levels safely above the threshold needed to prevent ovulation. The real culprit? Rifampin (brand name Rifadin) and its cousin rifabutin. These are enzyme inducers. They crank up your liver’s ability to break down hormones. Studies show rifampin can slash ethinyl estradiol (the estrogen in birth control pills) by 25% to 50%. Progestin levels drop too - by up to 37%. That’s enough to trigger ovulation. And yes, there are real cases of pregnancy in women taking rifampin for TB while on birth control. One verified patient reported exactly that on Healthgrades in 2022.What About Griseofulvin? (Yes, It’s Not an Antibiotic)
Griseofulvin is often grouped with antibiotics because it’s used to treat fungal infections like ringworm. But it’s not an antibiotic - it’s an antifungal. And it’s another enzyme inducer. Like rifampin, it speeds up how fast your body breaks down birth control hormones. The CDC classifies it as a category 3 interaction - meaning the risks outweigh the benefits. You need backup contraception for a full month after finishing griseofulvin. It’s rare these days, but if you’re prescribed it, don’t assume your pill is still working.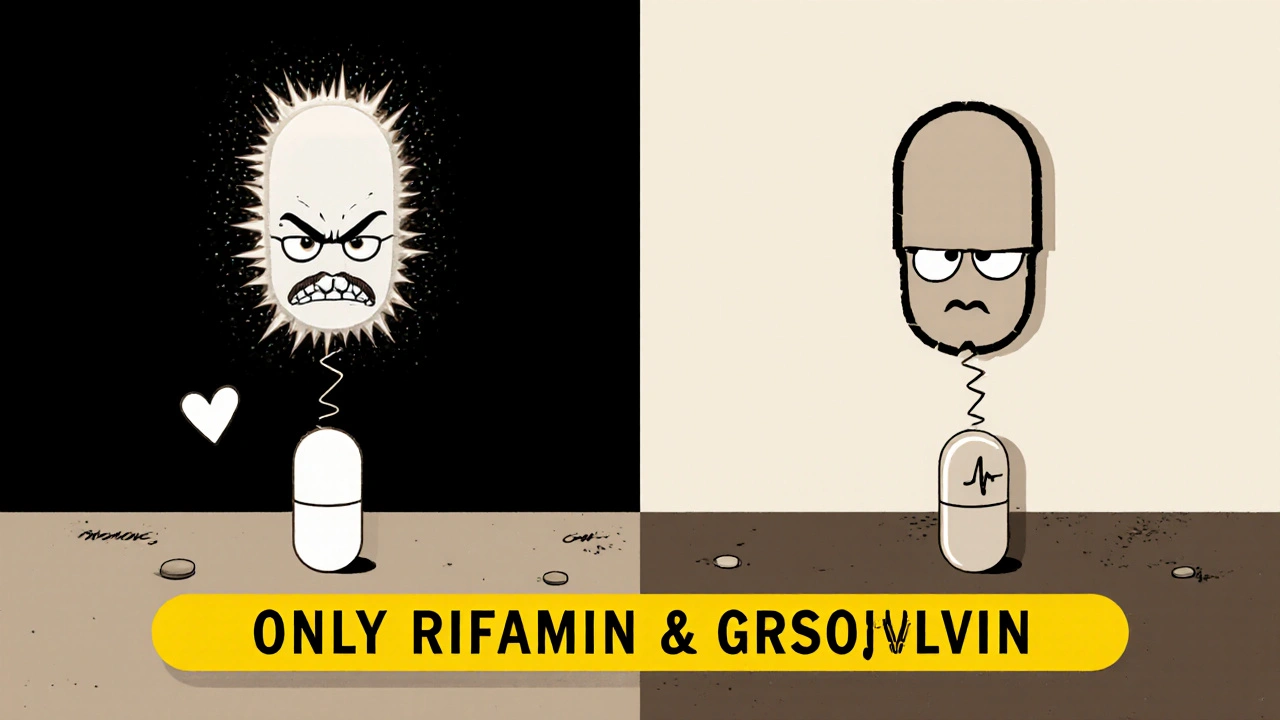
What About Other Drugs? (It’s Not Just Antibiotics)
If you’re worried about birth control failing, don’t just focus on antibiotics. Other common medications can do the same thing - and they’re often overlooked.- Lamotrigine (for seizures): At doses above 300 mg/day, it can lower estrogen levels.
- Topiramate (also for seizures and migraines): At doses over 200 mg/day, it interferes with birth control.
- St. John’s wort (herbal supplement): This popular remedy for mild depression can reduce estrogen by up to 57%, according to a 2017 study.
- Efavirenz and nevirapine (HIV meds): These antiretrovirals are known to reduce contraceptive hormone levels.
Why Do People Still Think All Antibiotics Are a Problem?
The myth persists because of bad science, fear, and overcautious advice. Early case reports weren’t controlled. They didn’t check what antibiotic the woman was taking. Many of the pregnancies happened because she missed pills, got sick, or took rifampin - but no one knew. The story stuck because it was simple: "Antibiotics ruin birth control." Easy to remember. Easy to warn about. Even today, 35% of pharmacists still recommend backup contraception for every antibiotic, according to a 2022 study in the Journal of the American Pharmacists Association. That’s not based on evidence - it’s based on habit. Some providers still say "just to be safe," even though ACOG’s 2022 guidelines say it’s not needed. Dr. Jen Gunter, an OB/GYN and author of The Menopause Manifesto, puts it bluntly: "There is zero evidence that common antibiotics like amoxicillin affect birth control." And she’s not alone. A 2023 survey of 500 board-certified OB/GYNs found 98% agreed: only rifamycins need backup contraception.What Should You Do?
Here’s the practical, no-fluff guide:- If you’re prescribed rifampin or rifabutin: Use backup contraception (condoms, diaphragm, or copper IUD) for 28 days after finishing the course. This applies to all hormonal birth control - pills, patch, ring.
- If you’re prescribed griseofulvin: Same rule. Use backup for 28 days after the last dose.
- If you’re prescribed any other antibiotic - amoxicillin, doxycycline, azithromycin, etc.: You don’t need backup. Your birth control is still working.
- If you’re unsure: Ask your doctor or pharmacist: "Is this an enzyme inducer?" If they say "no," you’re fine.
- Watch for rifaximin: It sounds like rifampin, but it’s different. Rifaximin (Xifaxan) treats traveler’s diarrhea and does NOT interact with birth control.

What If You’re Still Worried?
It’s okay to feel anxious. Hormonal birth control is important. If you want extra reassurance, using condoms during antibiotic treatment won’t hurt. But don’t assume you need to - especially if it’s not rifampin or griseofulvin. The risk of unintended pregnancy from amoxicillin or ciprofloxacin is no higher than if you didn’t take an antibiotic at all.What’s Changing Now?
In January 2023, the FDA updated the labeling for all hormonal contraceptives. The new labels now clearly state: "Rifampin, rifabutin, and griseofulvin may reduce effectiveness." And they add: "Other antibiotics do not affect effectiveness." That’s a big deal. It means drug manufacturers are now legally required to tell the truth - not spread fear. Research is also shifting. The National Institutes of Health now lists studying contraceptive effectiveness in obese patients as a priority. Why? Because women with a BMI over 30 already have a 2.5 times higher chance of birth control failure - regardless of antibiotics. That’s a bigger issue than most people realize.Bottom Line
The idea that antibiotics ruin birth control is outdated, inaccurate, and mostly false. Only two drugs - rifampin and griseofulvin - are proven to interfere. Everything else? Safe. Your pill still works. You don’t need extra protection. Stop worrying about amoxicillin. Start paying attention to the real risks: missing pills, vomiting, diarrhea, or taking drugs like St. John’s wort or certain seizure meds. If your doctor or pharmacist tells you to use backup for every antibiotic, ask them to check the CDC guidelines. They might be following old habits - not current science.Do antibiotics like amoxicillin make birth control less effective?
No. Amoxicillin and other common antibiotics like azithromycin, doxycycline, and ciprofloxacin do not reduce the effectiveness of birth control pills. Decades of research, including reviews by the CDC and ACOG, confirm this. Only specific enzyme-inducing drugs like rifampin and griseofulvin affect hormone levels.
Which antibiotics actually interfere with birth control?
Only rifampin (Rifadin) and rifabutin (Mycobutin) - used to treat tuberculosis - are proven to reduce birth control effectiveness. Griseofulvin, an antifungal used for fungal infections like ringworm, also interferes. All other antibiotics, including penicillins, macrolides, and fluoroquinolones, have no clinically significant effect.
How long should I use backup contraception after taking rifampin?
Use backup contraception for 28 days after finishing your last dose of rifampin or rifabutin. This applies to all forms of hormonal birth control - pills, patches, and vaginal rings. The CDC and ACOG both recommend this timeframe to ensure hormone levels return to protective levels.
Can I rely on my birth control if I’m on antibiotics for a UTI or sinus infection?
Yes. Antibiotics commonly prescribed for urinary tract infections (like nitrofurantoin) or sinus infections (like amoxicillin or amoxicillin-clavulanate) do not affect birth control. The CDC confirms that these drugs do not lower hormone concentrations to sub-therapeutic levels. No backup needed.
Why do pharmacists still tell me to use condoms with antibiotics?
Many pharmacists follow outdated advice or err on the side of caution. A 2022 study found that 35% of pharmacists still recommend backup contraception for all antibiotics, even though medical guidelines have changed. This is often due to fear of liability or misunderstanding the science. Always ask if the antibiotic is an enzyme inducer - if not, your pill is still working.
Does vomiting or diarrhea affect birth control more than antibiotics?
Yes. Vomiting within two hours of taking your pill or severe diarrhea can reduce absorption - more than any antibiotic. If you’re sick, follow the instructions on your pill packet: if you vomit, take another pill as soon as possible. If diarrhea lasts more than 48 hours, use backup contraception. This is a bigger risk than most antibiotics.
Is St. John’s wort dangerous with birth control?
Yes. St. John’s wort is a herbal supplement that strongly induces liver enzymes, reducing estrogen levels by up to 57%. It can make birth control ineffective. Even if you’re not on antibiotics, using this supplement while on hormonal contraception increases your risk of pregnancy. Always tell your doctor if you’re taking herbal supplements.
What about rifaximin? Is it the same as rifampin?
No. Rifaximin (Xifaxan) is used to treat traveler’s diarrhea and gut infections. Although it sounds similar to rifampin, it doesn’t get absorbed into the bloodstream the same way. The FDA confirms it does not interact with birth control. Don’t confuse the two names - they’re very different drugs.





Write a comment